When it comes to caring for children and young people in hospital, communication presents particular challenges, and getting it right for our young patients means getting it right for their families too. So how can we do this? Sarah Chapman hears from Anne and Sylvia, who share some experiences from their daughter’s and son’s time in hospital being treated for cancer, and looks at some evidence and resources.
Page originally published: 13 February 2015. Revised and republished: 15 August 2022, to include recent NICE guidance and other resources.
Take-home points
Jeri-Joann (J-J)
Anne is a nurse who experienced another side of health care when her daughter J-J had cancer. J-J was a young adult who had a mild learning disability. Anne explains,
“if you got into deep questions with her or asked her something, to figure something out, then… she would be lost and she didn’t want to admit that so she would just kind of ignore you or not answer and so that created problems. She knew this herself and so that was why she wanted me to make the decisions.”
Two years after J-J had a large fibroid removed, she had surgery for an aggressive ovarian cancer.
“In J-J’s mind she knew she had cancer, she knew she was really sick but also as far as she was concerned she was getting better… I know that was not the case but I supported her in that, as did her sister, because that was the best we could do for her, to support her. She only wanted the information she asked for and she didn’t want to make the decisions. She would say, “Ask my Mum, she will tell you”. She had a team in the cancer clinic… they accepted that, they worked with her.”
But this didn’t always happen and for Anne the gaps in communication were a big concern.
“A new oncologist came to work in the clinic and she didn’t know us, she didn’t know the background, didn’t really understand why when J-J was an adult she wasn’t making her own decisions and why I was making the decisions for her. But she was verbalising this in front of J-J and that was really upsetting for both of us.”
Another time, during a stay at her local hospital, J-J was seen by another doctor:
“Apparently he had come into the room and, again, you know, she was an adult, and he figured she was making the decisions and he read from her chart the diagnosis that she was a terminal patient and dying and this is what they were doing. And he read that to her. He read from her chart the diagnosis that she was a terminal patient… and he read that to her. Well, she was, needless to say, just beside herself, so I went up to the desk and asked the nurses “Where is the doctor” – “He is making rounds” – and I said, “Well I want to see him” – “He is making rounds” – “I don’t care what he’s doing, I want to talk to him and I want to talk to him now”. So I explained to him and said, “I don’t care what you do or how you do it but you go into her room and you talk to her and sort it out and settle her down so that she is back where she was when you entered the room”. So he did. He went in and he talked to her and said he was sorry that he’d read from the chart and had misread it and had made a mistake there and he was sorry and that they would sort it all out. When she went in for the last four days of her life, it was the same doctor taking care of her and the change was, well, he was excellent, I have to say.”
Anne concludes:
“One of the things that is really crucial in health care is to always have the perspective, whether you call them patients or clients or consumers, citizens or whatever your term is, to have their perspective and viewpoint and things. Because it’s often very different from the provider perspective and you really need to have both of them before you move anything forward.”
Anne hopes that other parents who see the video will feel encouraged to speak up for their child’s needs and wants.
Matthew

During my time nursing children and teens with cancer, I became particularly close to Matthew and his family through his months of treatment. Matthew died just short of his 18th birthday, an anniversary shared with his mum Sylvia. We became – and stayed – friends. Sylvia has kindly shared her thoughts about communication through Matthew’s illness.
Matthew came to us only after a long period of misdiagnosis. Sylvia recalls:
“The surgeon said “you will not have heard of this Matthew. You have Non-Hodgkin’s Lymphoma.” Matthew said “I have cancer then.” A close friend of ours had been treated for the disease so we knew exactly what it was. I would have collapsed were it not for my amazing son being extremely brave and I had to be brave for him.”
At 17, Matthew might have been admitted to an adult ward.
“Fortunately for us, compassionate Dr K was happy to keep him under her care [on the children’s ward]. This proved to be the best possible thing for us, not only for Matthew and I but for his older brother and sister. Matthew was the ‘big boy’ there and the other children would spend time with him and looked up to him and I know this helped Matthew.
He was always very positive that he would get better. As long as ‘Mum’ was coping, everything was ok.
From the day Matthew was admitted, the communication was excellent. We were given leaflets to read, but I didn’t read them. We sat with Nurse A and she explained exactly what his treatment would be, including the side effects, which she did in a very compassionate way, answering any questions we had. Andrew [Matthew’s brother] was my rock and would ask the doctors questions I was never brave enough to ask for fear of the reply.
For the last ten weeks of his life, we all stayed there as a family. There were four wonderful nurses who Matthew grew very fond of, as did I. Always there for us on good and bad days for comfort and support… especially Nurse S, with whom Matthew had a great affinity. It was as though she had been assigned to us and us alone.”
It’s the little things…
Sylvia reminds us that how we make people feel often lasts longer than the details of what we say. What’s more, Sylvia’s and Anne’s experiences show that information isn’t always what is most needed or wanted and that it’s vital that we strive to put good communication, based on the needs and preferences of each patient and their family, at the heart of compassionate care.
Communication is, of course, so much more than words. Sylvia and I recalled with some amusement that on one occasion in Matthew’s last weeks, when she appeared at his bedside, Matthew remarked “Mum, you don’t look attractive enough!” Sylvia had not taken her usual care with her appearance and this rather frightened Matthew, who really needed to know that Mum was ok.
Evidence and resources
Cochrane evidence
The Cochrane Review Interventions for promoting participation in shared decision‐making for children with cancer (published November 2016) addressed ways of involving children with cancer in decisions about their care but found no trials that could be included. This is a lamentable gap in the research. The reviewers comment that
“Much of the evidence promoting children’s participation is authored by policy makers and we lack strong evidence from research that supports these recommendations. It does seem to be the ‘right’ approach for clinicians to include children in SDM [shared decision-making] but we do not have strong evidence that indicates which children desire inclusion, at what point in the trajectory of their treatment or illness, and with whom do they want to share decision-making and about what topic. Children sometimes prefer a passive role in SDM because they are too ill or distressed by the treatments. Likewise some children prefer to hear information from their parents especially if it is ‘bad’ news or about treatment side effects.”
NICE guidance
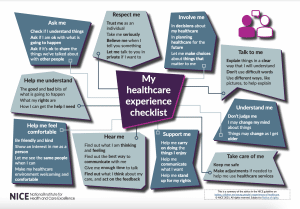
Young people were involved in the development of The National Institute of Health and Care Excellence (NICE) guideline on Babies, children and young people’s experience of healthcare (published 25 August 2021).
Me first
Me first is an education and training resource that helps health and social care professionals to develop their knowledge, skills and confidence in communicating with children and young people. It has been developed by Great Ormond Street Hospital and Common Room Consulting in partnership with health and social care professionals and children and young people.
Me first has a Resources hub.
One of these is Teens in Hospital, is a booklet written by 17 year old Jessica Platt after her stay in hospital, being treated for pneumonia. Jessica noted a “gap in the confidence of many members of the clinical staff when it came to interacting with me”. She surveyed teens and doctors, found out more about teenage brains and drew on her experience to produce this booklet of tips on “how to talk to us teens in a way that we will (hopefully) listen to”.
Our thanks to Anne and Sylvia for sharing their stories.
Sarah Chapman has nothing to disclose.



Hi Sarah
I was wondering if you have more information on how I can or my daughter can volunteer to spend time with young people in hospital. I tried contacting some in my area of Manchester but seems to get back any response. Thank You.
Exbia
Hi Exbia,
I’m not knowledgable about this, but hospital trusts do advertise opportunities on their websites, so that’s all I can really suggest.
Best wishes,
Sarah Chapman
Agree this is such a crucial topic – it’s something of an indictment anyway that young people requiring treatment so often have to be placed in settings that are either way too young, or way too old, to meet their social and emotional needs. It almost seems the least care providers should do is to give thought to how they communicate in an appropriate way and involve young people in their own care. This can be compounded further where young people with learning difficulties – for example, autism – require hospital treatment. Staff receive little training and often have very limited knowledge of these conditions. It is so important to remember it’s an individual who is being treated, not simply a condition or an illness.
Thank you for your comments Tracey, and I quite agree!
Sarah
It is so important that we get this communication right. Our family had a five year path through incredibly intensive surgery & cancer treatment for a cancerous brain tumour which unfortunately (words fail me) ended up with our 16 year old dying at home during London 2012. So I saw a lot – parents need a lot of help not only processing information themselves but in communicating it in a way that their own child needs. I realised that lying even for the best reason – I want to protect my child – is still a terrible idea if your child then does not trust you and might then refuse to continue the horrendous treatment, which then puts their life at risk. In microcosm, the classic example of this is to say, when your child asks if an injection is going to hurt, “No”. I heard this so many times. It was much better to say it will be a very quick hurt but the medicine is helping to make you better. It gets particularly difficult when treatment fails and the medical team and the child/young person and family need to make decisions about end of life care. Messy is the word! But if it is done well – and 5 years down the line we had got better at shared decisions with our son – there is nothing in my life that will ever give me as much consolation as knowing our son had a good death, one that he wanted and we enabled. Good Luck.
Thank you for sharing this Sacha. I’m sure many other parents who have experienced supporting their child through cancer treatment will agree with you on this, and indeed parents of children undergoing treatments for other things. As nurses we were taught that honesty is the best policy, and certainly about what procedures are like, but Anne’s story is a reminder that health professionals need to be sure to listen to the family to help them ‘get it right’ in terms of communicating well with their young patient. You’ve reminded us too that families need support in both processing and sharing information in ways that are right for their child.
I know you are working hard campaigning for HeadSmart, raising awareness of brain tumours in children, and wish you well with that.
Sarah