In this short blog, Professor Martin Burton looks at the evidence on ear drops for removing earwax, and some things to think about, including whether you need to remove it at all. Professor Burton is an ear nose and throat doctor and an author of the Cochrane Review on ear drops to remove earwax.
The blog is based on an earlier version published 26 July 2018. It has been substantially revised and republished 24 March 2023
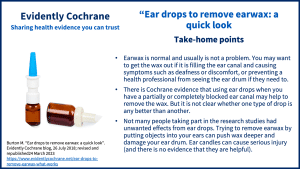
Take-home points
The evidence comes from a Cochrane Review* and is relevant to adults and children.
When is earwax a problem?
Earwax is normal. It is produced by glands in the outer part of your ear canal. In most people, most of the time, it is not a problem. But not always. Usually the wax passes out, along the ear canal, into the bowl of the ear; it doesn’t produce any symptoms, and doesn’t ‘build up’ in any way.
But if it does build up to such an extent that the ear canal is blocked, it can produce some degree of deafness. If there is a lot of it, and it is hard and completely fills the canal, it is sometimes referred to as ‘impacted’ wax. In either of these circumstances, or if the wax is causing symptoms of pain or discomfort, it is probably worth doing something to try and get the wax out. Another reason for wanting to do this is if it is simply blocking the view of your ear drum. Sometimes a health professional needs to see the drum to help make a diagnosis. If there is too much wax in the ear canal they may not be able to do this – hence the need to get the wax out.
How is earwax removed?
Softening the wax with ear drops may be enough to allow the natural processes of elimination to occur so that the wax comes out of the ear on its own. Just like it should do. So, if time allows, simple softening and a ‘wait and see’ approach may be enough.
But if this doesn’t work, or there is no time to wait, your pharmacist or GP may suggest that you have the wax removed. This is usually done by a health professional. In these circumstances, they will often suggest that you use drops first (at least for a few days) to try and soften the wax before the removal is done. There are several benefits of this; it might lead to you not needing removal at all, or it may make the wax removal easier.
Various liquids can be used as ear drops include oils (almond or olive) and oil-based compounds, water-based compounds, or water by itself.
Ear syringing with water
When we talk about “having the wax removed by a health professional” what do we mean? In the past, this almost always meant having your ears ‘syringed’. This involved a health professional squirting warm water into the ear with a large syringe. The aim of this was to flush the wax out. But this system could only work in certain specific circumstances. The idea was that the jet of water from the nozzle of the syringe went past a lump of wax, hit the ear drum, bounced off the ear drum, and then – on its way out of the ear canal, the stream of water would carry the wax with it.
It’s obvious from this description that two things are critically important. The first is, there has to be a gap between a lump of wax and the walls of the ear canal. Otherwise, the jet of water simply drives the wax further inwards, and that can be a problem. Secondly, the ear drum has to be intact, and normal. If there is a hole in the ear drum, or the drum is missing completely (as can happen) the jet of water just goes through the hole and the patient can end up with an ear infection. Although syringing was once done a lot, usually by a nurse or doctor in primary care, there were always potential problems and risks associated with it. As a result, it is not often done nowadays, but can still be effective if done carefully, and safely, by an experienced operator.
“Micro-suction”
The main alternative to syringing is often referred to as “micro-suction” or “suction cleaning”. Using a special sucker, and some form of magnification (either a large microscope or a special set of magnifying spectacles) with the patient either lying down or sitting, a health professional will suck wax out of the ear. They may also use very fine instruments to lift or tease it out.
There is a general agreement that this may be easier to do if the wax is softened first with ear drops. So you may be asked to use drops for a few days before having this done. Like most things, this procedure needs to be done carefully, with good quality equipment by someone properly trained and experienced in doing it. In those circumstances, it can often be done without undue pain or discomfort and without causing any damage to the ear canal or ear drum. But even in the best hands, it can be tricky and the ear canal skin can be grazed.
All hospital ENT departments have the equipment and skills to do micro-suction but not all are able to offer the service to the general public. Some GP practices also do it and – increasingly – it is being offered by private providers (sometimes in association with hearing aid provision).
Making a choice about treatment? Think BRAIN!
It can be helpful to think BRAIN: What are the Benefits, Risks, Alternatives, what do I want and what if I do Nothing?
What are the benefits of using ear drops and how do different types compare?
The evidence in our Cochrane Review suggests that using something other than just water when you have a partially or completely blocked ear canal may help to remove the wax. But it is not clear whether one type of drop is any better than another, or whether drops containing active ingredients are any better than plain or salty water.
What are the risks of ear drops?
Any treatment can have unwanted effects.
Not many people taking part in the research studies had unwanted effects from ear drops and these were mild, such as slight irritation or pain or unpleasant smell. Every so often we come across a patient who is sensitive or allergic to one of the chemicals contained in some drops. This is more likely when the drops contain active compounds or preservatives. So this doesn’t happen with plain water drops.
What are the alternatives?
Trying to remove earwax by putting objects (including cotton buds) into your ears can push wax deeper and damage your ear drum. Ear candles can cause serious injury (and there is no evidence that they are helpful).
What are your preferences?
If you’ve used ear drops before to soften ear wax, you might want to use the same again or try something different. Cost and availability may also be relevant.
What if you do nothing?
In our Cochrane Review, we did not find any evidence to tell us whether using water or saline (salty water) was better than doing nothing.
Find out more
*The evidence comes from this Cochrane Review:
Aaron K, Cooper TE, Warner L, Burton MJ. Ear drops for the removal of ear wax. Cochrane Database of Systematic Reviews 2018, Issue 7. Art. No.: CD012171. DOI: 10.1002/14651858.CD012171.pub2.
- NHS Earwax build-up
- NHS Inform Scotland Earwax build-up
- RNID Ear wax build up
- NICE clinical knowledge summary – Earwax
More about hearing conditions
On this page Hearing conditions: evidence, experience and resources (March 2023) we share trustworthy evidence and resources about hearing conditions and highlight opportunities to take part in research. Our blogs help to set evidence in context and make it easy to understand, and often include reflections from people living with hearing conditions and from health professionals and researchers.
Join in the conversation with @SarahChapman30 @CochraneUK @CochraneENT @martinjburton or leave a comment on the blog.
Please note, we cannot give specific medical advice. We do not publish comments that link to individual pages requesting donations or to commercial sites, or appear to endorse commercial products. We welcome diverse views and encourage discussion. However, we ask that comments are respectful. We reserve the right to not publish any we consider offensive. Cochrane UK does not fact check – or endorse – readers’ comments, including any treatments mentioned.
Martin Burton has nothing to disclose.



Hello,
Enjoyed your article on removal of earwax. Can you do a review on hearing aids?
Thank-you.
James
Hello, we have a blog coming soon that will bring together our multiple blogs on hearing conditions, evidence and resources. There is a Cochrane Review on hearing aids https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD012023.pub2/full
Best wishes
Sarah [Editor]
Hello James, you may be interested in our new blog ‘Hearing conditions: evidence, experience and resources’: https://www.evidentlycochrane.net/hearing-conditions-evidence-experience-and-resources/
– Selena [editor]
[…] as this usually just pushes earwax further into your ears). To get rid of excess earwax, consider buying eardrops from your local pharmacy. Professional ear cleaning could be another option, which may involve […]
I have only 60% hearing in one ear.totally deaf in the other,I’m totally astounded what I am reading,and what people are putting into their ears! For gods sake go to your GP!
You are absolutely spot on. So dangerous to be poking about or introducing solutions to such a delicate area without a Doctor’s advice.
What can l do my ears are broked can’t …they broked more after trying to soften the wax using oil.
Hello Evelyn,
It may be best that you speak to a pharmacist first of all, especially if you are concerned that your ears might have become worse. You can find some useful information on the NHS Choices website: https://www.nhs.uk/conditions/earwax-build-up/
With best wishes,
Selena [Editor]
For anyone like myself who finds the glycerol/hydrogen peroxide
solutions helpful
Earex Advanced. Sole ingredients Glycerol, Hydrogen Peroxide 5%
12ml costs around £4.50 from most outlets
Glycerol and Hydrogen Peroxide 6%, 200ml bottles cost around £2 each
from Boots
The only question is the exact proportions to use. Which is how I happened
to come across this blog.
i have lost all of my earwax in my left ear and developed dermatitis. Now when I use the derma creams they go straight into my mouth leaving me with a sore throat on the left side. on consulting three doctors they each said that this cannot happen.
This situation came about when I was told by the chemist to use olive oil. What should
I have tried everything but still no relief in my left ear…Was tested for an infection but it was negative..Waiting to see if they will try to syringe my ear again..My gp surgery does not do it anymore. I am becoming desperate now as I have no hearing in my ear..This has been going on for 6 months now.
Hi
I first noticed my tinnitus about 30yrs ago and i think it causes a build up of wax which doesn’t help. In the last 5 years ive wasted about £100 on useless gadgets & liquids. I have hard stubborn wax deep in ears & my left ear is worse (i can tell by pinching my nose & blowing which temporarily improves hearing in right ear). Any impartial advice would be appreciated.
thanks
I am a pro violinist and have a moderate hearing loss in the upper range although the violin is so close to your ears that it does not prevent me in my work. Hearing aids are no good for playing as they distort the sound. I tried olive oil drops as I had a problem with hardened earwax rattling in my head but it is so messy and the oil seems to get everywhere. Earex after just one treatment improved the sound of my violin’s high notes so I will continue with that.
Had my ears shrynged last week but it’s made no difference my ear canal is very tiny what can I do to dissolve it