In this blog for nurses, Sarah Chapman looks at Cochrane evidenceCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. on intermittent catheterisation for long-term bladder management and Sharon Eustice, a Nurse Consultant championing bladder and bowel health across Cornwall and the Isles of Scilly, reflects on its implications for practice and future research.
Blog updated on 29 October 2021 and last checked 21 March 2023
What is intermittent catheterisation?
Intermittent catheterisation (IC) involves passing a catheter into the bladder to drain the urine, and then removing it. It is advocated as an effective way of managing the problem of incomplete bladder emptying.
IC can be done by many patients themselves, including children and the elderly, or their carers. How often it’s done will vary, but a general principle for adults is to catheterise often enough to avoid having more than 500ml of urine in the bladder.
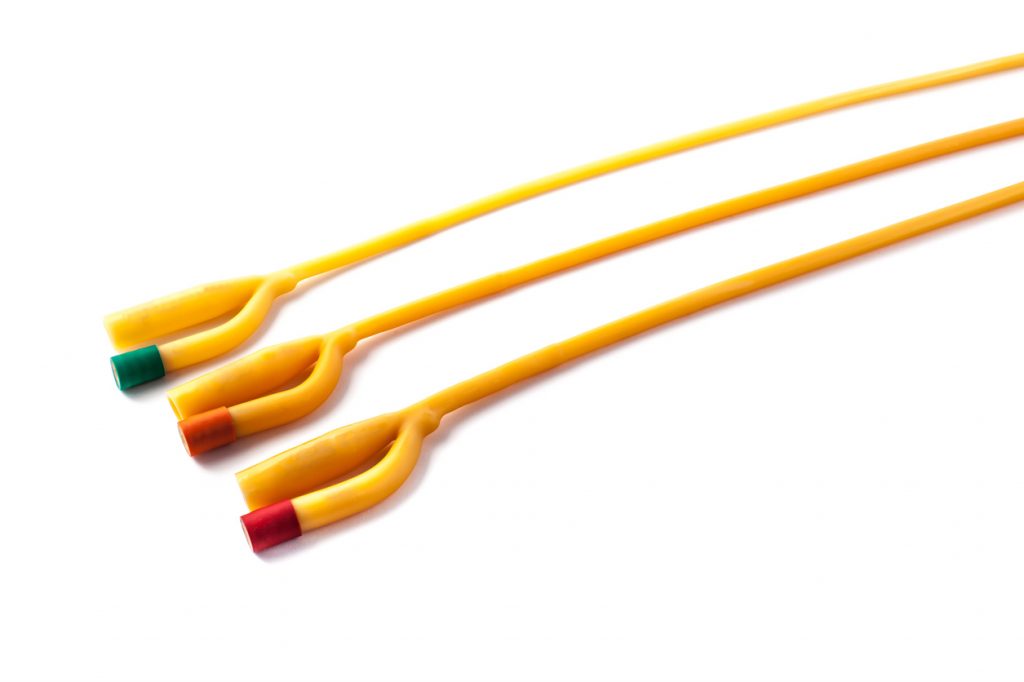
There is a wide variety of catheter types for IC, from plain uncoated catheters, which may be used with or without lubricant, cleaned by a range of methods, and reused; to coated catheters, which are for single use only. Coatings vary and some catheters come pre-lubricated and with an integrated drainage bag.
Benefits and harms of intermittent catheterisation
The benefits of IC include a reduced riskA way of expressing the chance of an event taking place, expressed as the number of events divided by the total number of observations or people. It can be stated as ‘the chance of falling were one in four’ (1/4 = 25%). This measure is good no matter the incidence of events i.e. common or infrequent. of problems associated with indwelling catheters such as damage to the urethra or bladder neck, reduced need for equipment, and potentially fewer urinary symptoms, such as urgency, between catheterisations. Not having a catheter in place all the time has advantages in terms of what the person is able to do, including greater freedom to express their sexuality.
Urinary tract infection (UTI), a potential hazard of any type of urinary catheterisation, is the most common harm, and prostatitis is a risk for men.
Evidence to inform choices about intermittent catheterisation?
It would be helpful to have reliable evidence to help guide choices about intermittent catheterisation, including the catheter type, the method of catheterisation, and other factors such as catheter reuse. What impact do they have on complications? What do people prefer? How easy are they to use? How cost-effective are they?
The Cochrane Review Intermittent catheter techniques, strategies and designs for managing long‐term bladder conditions (most recently version published in October 2021) brought together the best available evidence on IC for long-term bladder management, from 23 trialsClinical trials are research studies involving people who use healthcare services. They often compare a new or different treatment with the best treatment currently available. This is to test whether the new or different treatment is safe, effective and any better than what is currently used. No matter how promising a new treatment may appear during tests in a laboratory, it must go through clinical trials before its benefits and risks can really be known.. What they found was essentially a big evidence gap.
There were lots of problems with the trials, including small sample sizes, sparse dataData is the information collected through research. on adverse events and no usable data on cost-effectiveness. The review authors conclude “it remains unclear whether the incidenceThe number of new occurrences of something in a population over a particular period of time, e.g. the number of cases of a disease in a country over one year. of UTI or other complications is affected by use of aseptic or clean technique, single (sterile) or multiple‐use (clean) catheters, coated or uncoated catheters or different catheter lengths.”
Given the lack of reliable evidence to inform decisions about intermittent catheterisation, where does this leave practitioners and patients needing to make choices? Over to Sharon.
Intermittent catheterisation: helping your patient make choices
When the patient and their health care professional have confirmed that IC is the best option to care for their bladder, choosing the best catheter may not be easy. This is because there are several catheters available on prescription to choose from. The fundamental concept of all the catheters is that of a hollow tube which can drain urine from the bladder. What varies is the size of catheter, its length, how it is prepared ready for use, the style of packaging and ease of carrying it around.
Without reliable evidence to help us, choices must be based on other factors.
It is important to allow enough time to discuss the role and procedure of IC. For many there will undoubtedly be worries about using the procedure. However these worries are usually settled with good information, along with sensitive and positive communication. At this stage, most patients don’t feel ready to choose their own catheter, but need guidance on which one to start with.
Considerations for guidance include dexterity, visual impairment, positioning for IC and any anatomical aspects (e.g. prolapse). Discussing these aspects will help identify what catheter is best to start off with, whilst always bearing in mind individual patient preferences.

As they begin to master the procedure, their confidence grows and knowing what catheter may suit them tends to emerge.
Most patients choose a single use catheter, where a new catheter is used each time. Indeed, the NHS has predominantly guided patients to this type of catheter also. However, there is growing interest in the reusable catheter, which used to be very popular, but the single use catheter pushed it aside.
More research into the types of catheter (single use or reusable) is needed so that we can address what might work best for people’s lifestyle. For example, how best to clean the reusable catheters in between use is a key area to clarify
Intermittent catheterisation can offer significant clinical benefits to bladder symptoms and restore quality of life. Importantly, the patient (and/or carers) need regular follow-up and good access to their healthcare professional to seek clarity on any new concerns and check that all is well. There are occasions when the regime of IC needs adjusting to fit the dynamic nature of the bladder.
Where does this leave us?
IC has the potential to offer significant therapeutic benefits and improved quality of life. Despite a lack of reliable evidence, we need to continue offering IC where clinically appropriate and safe to do so and to make decisions with patients based on other factors. Future research needs to address the gaps, adopting the highest standards of design, methodology and reporting, and addressing outcomesOutcomes are measures of health (for example quality of life, pain, blood sugar levels) that can be used to assess the effectiveness and safety of a treatment or other intervention (for example a drug, surgery, or exercise). In research, the outcomes considered most important are ‘primary outcomes’ and those considered less important are ‘secondary outcomes’. that matter to patients, so that there is reliable and relevant evidence to help with decision-making.
Key points
- There is no reliable evidence to inform decisions about intermittent catheterisation
- Effective communication between the patient and healthcare professional is fundamental to improve the patient experience
- Patients should be provided with enough information about IC before making any decisions about their care
Sharon Eustice and Sarah Chapman have nothing to disclose. Views on practice are Sharon’s own.
Prieto JA, Murphy CL, Stewart F, Fader M. Intermittent catheter techniques, strategies and designs for managing long‐term bladder conditions. Cochrane Database of Systematic ReviewsIn systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. 2021, Issue 10. Art. No.: CD006008. DOI: 10.1002/14651858.CD006008.pub5. Accessed 29 October 2021.
Find out more about the work of Cochrane Incontinence here and find them on Twitter @C_Incontinence


