In this blog, Sarah Chapman, whose Mum died during the first lockdown, reflects on the text conversations she had with her Mum’s carer about her dying. She also talks about recent evidence on effective communication between health professionals, those who are dying and their families and about our need for knowledge of ordinary dying when many of us don’t witness a death until we are older adults ourselves. The blog also contains sources of information and support for non-medical people and health professionals.
Page last updated 18 September 2023
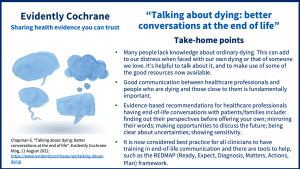
Take-home points
My lovely Mum, Marian, died in both ordinary and extraordinary circumstances. An ordinary death, peacefully at home, as was her wish. So lovingly cared for by Sylvia, her live-in carer (a retired nurse), and another much loved helper, Joanne. An extraordinary death, on 12 April 2020, at the height of the first lockdown. No visitors allowed. No family to attend Mum’s dying. It was Joanne who held Mum in her last lucid moments and Sylvia who sat with her in her final hours. An extraordinary, ordinary death.
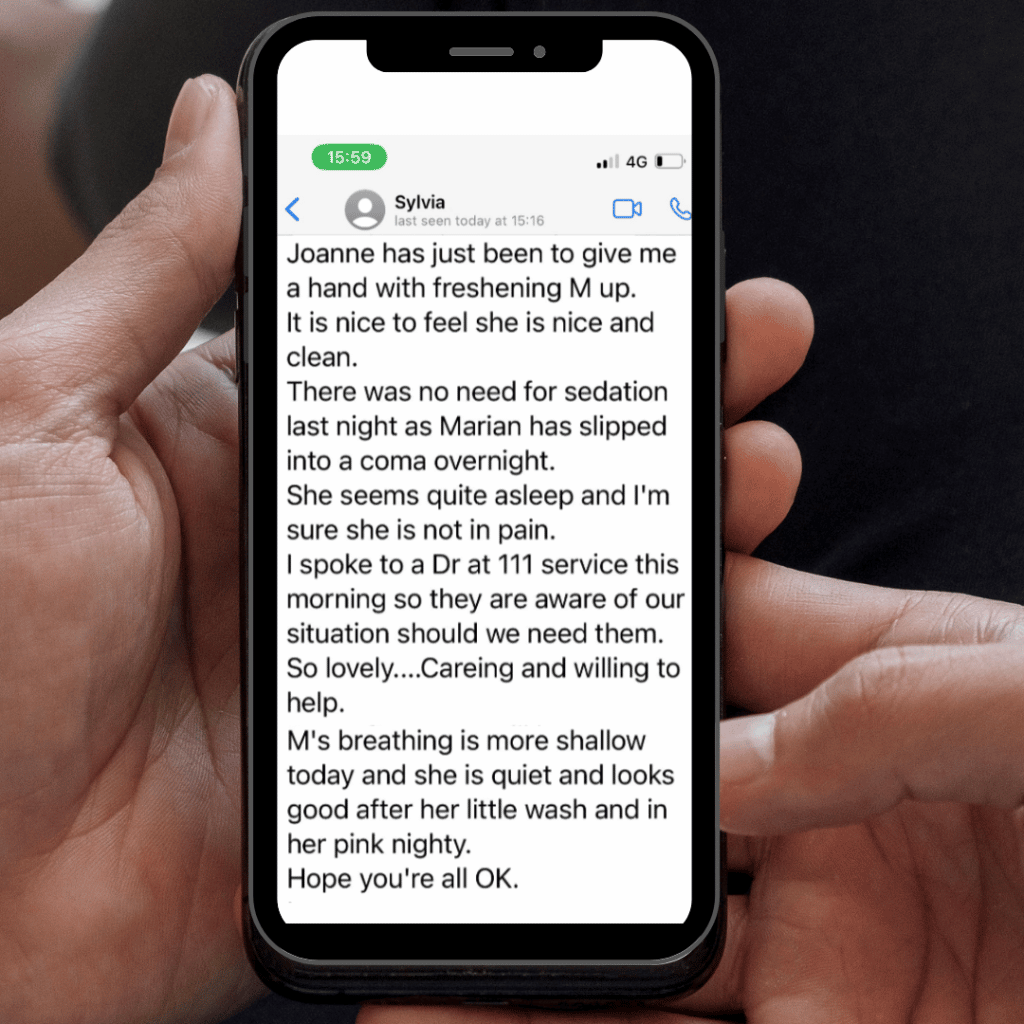
Sylvia had to communicate with me about Mum’s dying by text messages (I’m too deaf for phone calls), and I have these still. I have reflected since on how skilfully, and how tenderly, she did this, and how important that was for me and my family.
Mum went downhill quite rapidly, after years of decline with Alzheimer’s, and it was by text that Sylvia had to convey the changes. By text, she told me how she and Joanne were caring for her; about support from the GP and community nurse, and about little things that mattered to us (“She seems quite asleep and I’m sure she’s not in pain… She looks good after a little wash and in her pink nightie”). We exchanged memories of Mum, when I told her I was making biscuits from Mum’s recipe as a way of feeling close to her. She got it just right when suggesting it would be wise to choose a funeral director. I told her it was ok to send me news of Mum’s death by text… At every step she was clear and oh so gentle.
To do all this by text, and for none of us to be with Mum, were things we wouldn’t have imagined. But it seems to me that there are key things here that Sylvia did that would have been important however we were communicating.
Sylvia helped us to understand that Mum was dying and shared how she expected this to be. She kept us up to date with how Mum was and how she was being cared for. She gave us confidence that Mum was as comfortable as possible, that she wasn’t alone, and that her wishes for the end of her life (including those captured in an Advance Decision) were being upheld. She kept Marian the person present in our exchanges and never reduced her to tasks or problems. Importantly, Sylvia was clear and kind, and we trusted her absolutely.
Can evidence tell us what makes for good communication at the end of life?
We don’t need science to tell us that good communication makes an important difference to people at the end of life – their own dying or that of someone they love. But can it help us know what the crucial elements of that communication are?
The new Cochrane Review on Interventions for interpersonal communication about end of life care between health practitioners and affected people (published July 2022) finds only “inconclusive” evidence on the effects of interventions aiming to improve communication between health professionals and dying people and those close to them.
However, a non-Cochrane rapid review Communicating with patients and families about illness progression and end of life: a review of studies using direct observation of clinical practice (published December 2021) perhaps gets us somewhere. It includes evidence from studies where real conversations about illness progression and end of life, from a variety of settings, have been analysed. From this, the authors have developed five key recommendations for clinicians who need who need to discuss illness progression and end of life with patients or their families:
- Ascertain a patient or family member’s perspective before offering your own
- Where possible, mirror the language of the patient or family
- Create opportunities to discuss the future
- Be clear about uncertainties
- Display sensitivity
The authors say this review strengthens and expands existing evidence but that further research is needed to understand ways clinicians explore options with patients and families.
It is now considered best practice for all clinicians to undertake training to embrace these issues and develop a good relationship with the patient and carer. For instance, in Scotland doctors have developed a framework to promote sensitive conversations: RED-MAP.
We need to talk about dying
Let’s all help ourselves by talking about dying, and especially ordinary dying. We all need to know what this is, what it involves for the many of us who die after the years or illness finally catch up with us. Unlike previous generations, many of us won’t experience death up close until our parents die, often when we are in, or beyond, middle age. Our ignorance is hurting us. It sets us up for fear and distress, misunderstanding what our loved one is going through. It means we have more uncertainty than we need to have.
As palliative care doctor Kathryn Mannix says in this excellent short video “Dying is not as bad as you think”, we’ve lost the rich wisdom of normal human dying – and we need to reclaim it. Here, she explains the gentle process of normal dying. What a difference it makes to know that the “death rattle” (sounds made by a dying person breathing through mucus and saliva in their throat that they no longer clear or swallow) isn’t something terrible, but a sign that the person is so deeply relaxed, so deeply unconscious, that they don’t feel the tickle of saliva at the back of their throat. Nor do we need to be distressed about our loved one no longer eating or drinking. As Dr Mannix explained in this Twitter thread, “although we don’t eat when we’re dying, that isn’t the same as starving… A dying person uses very little energy & has very low need for calories… Feeding tubes would deliver food into a gut that isn’t functioning. Little gets absorbed, most runs through as diarrhoea, regurgitates back or causes cramps: not a helpful thing to do.”
As a former nurse, I knew more about dying than many and drew on this knowledge when Mum was dying. But Sylvia’s clarity about what was happening, and how she expected things to go, particularly helped my daughter, and her excellent, sensitive communication helped us all.
We can also all help ourselves by having conversations about dying and by finding out more. I’ve included some resources I think are useful below – and with thanks to Professor Scott Murray for his suggestions.
For more information and support
Resources for health professionals:
- RealTalk is a new, evidence-based initiative comprising Resources, Events and Consultancy based on authentic recordings of real-life health care, and robust scientific evidence about healthcare communication.” RealTalk resources are available free of charge to registered professionals and trainers working in the NHS, organisations that work with the NHS (e.g. hospices), and higher education institutions.
- Support Around Death
- RCGP Palliative and End of Life Care Toolkit – Toolkit for healthcare professionals to support patients nearing the end of life to live well until they die.
- RCGP Talking about dying 2021: how to begin honest conversations about what lies ahead
- The Palliative Hub Professional (Ireland & UK)
- The Serious Illness Conversation Guide
- Four Questions to Start Serious Illness Conversations for Clinicians
- End-of-life essentials (an education module for healthcare professionals, from Australia but available to HCPs in the UK).
- Lancet Commission on the Value of Death and see also https://valueofdeath.org
Resources for everyone:
By Kathryn Mannix:
- Books – ‘With the End in Mind: How to Live and Die Well’ and ‘Listen: How to Find the Words for Tender Conversations’.
- Podcast – The Art of Dying Well, episode 28 The Art of Listening Well
- Short videos:
- Food for Thought (with Dr Jared Rubenstein)
- End of the Line (with Dr Jared Rubenstein)
- “Dying is not as bad as you think” and What happens as we die? (watch below)
Kathryn Mannix has also explained here about ‘terminal agitation’ (muddled thinking with unusual behaviours in a person close to death).
Short videos from the University of Edinburgh:
- How to live and die well: understand what might happen and plan. This short video is for everyone, explaining illness trajectories. It’s to help people who are currently well to think ahead. It is also for people who currently live with progressive illness. It’s also for family members and carers of those who are ill, and who want to learn what can happen in the future so they can plan ahead.
- Strictly Come Dying. This light-hearted video discusses the different illness trajectories as though each were a dance with a particular tempo and complexity. Just as knowing the different dance steps will help someone dance well, understanding typical physical and emotional sequences of various illnesses can help people live and die well.
From HealthTalk
Living with dying – “you can find out about the experiences of living with a terminal illness by seeing and hearing people share their personal stories on film.”
Public information websites about care planning, serious illness, death, dying and bereavement:
- Patient Information: Serious Illness Conversations
- NHS Inform – thinking and planning ahead (NHS Scotland)
- Dying Matters (England)
- Good Life, Good Death, Good Grief (Scotland)
- Marie Curie – care and support through terminal illness (UK)
- Macmillan Cancer Support – cancer information and support (UK)
- Age UK – information and advice (UK) and end of life issues
- End of life – useful organisations (a list from Alzheimer’s UK)
Related Evidently Cochrane blogs:
Communication with cancer patients: does practice make perfect?
Tube feeding for people with severe dementia: making decisions
Glioblastoma: honest conversations for shared decision-making
Join in the conversation on Twitter with @CochraneUK @SarahChapman30 or leave a comment on the blog.
Please note, we cannot give specific medical advice and do not publish comments that link to individual pages requesting donations or to commercial sites, or appear to endorse commercial products. We welcome diverse views and encourage discussion but we ask that comments are respectful and reserve the right to not publish any we consider offensive. Cochrane UK does not fact-check – or endorse – readers’ comments, including any treatments mentioned.
Sarah Chapman has nothing to disclose.


Unsatisfied
Just before I die
I’d probably cry.
Yes! I wouldn’t lie
With a terse, ‘goodbye’,
Feigning completion –
Full satisfaction;
The long due demise
Of a fellow, wise.
Boghos Artinian
There is such a thing as a good death, and I’m so touch by your account of your mum’s good death, Sarah. My lovely little mum, Marie, died immediately before lockdown. She had suffered in pain and fear for several weeks in a hospital spread to thin to provide anything but the most basic care – and often not even that. My sisters and I stayed by her side to advocate when she needed her palliative pain meds, when her blood ox dropped too low, when her NG tube was blocked. When the hospital failed to arrange patient transport to hospice care, my sisters and I did a ‘prison break’ and drove my mum there ourselves: complete with oxygen tank, IV, NG tube and catheter. The contrast between hospital and hospice care was astounding. The hospice welcomed my mum with such care and comfort. They cared for our whole family as she slipped away. How I wish I’d had your blog back then
Thank you Kate for taking the time to write here and share your experience about your lovely mum. I’m so sorry, though, that she suffered in hospital. I hope there is some comfort for you and your sisters in knowing you were there for her and advocated for her – I’m sure you will have made a difference, both in the loving companionship you provided for your mum – and each other – at such an awful time, and in helping her get what she needed, even down to the ‘prison break’. Thank goodness your mum was able to end her days in the hospice and that you all benefited from their excellent care. I didn’t talk about it in the blog but Atul Gawande, in his excellent book ‘Being Mortal’ says that “Endings matter, not just for the person but, perhaps even more, for the ones left behind.” So true. I hope that the care and comfort given your mum, at the end, and by you and your sisters throughout, is helping as you grieve for your mum.
Very best wishes,
Sarah
Dear Sarah, Thank you for sharing your story. I am so sorry for your loss. This piece is very touching and includes many helpful resources. I enjoyed Dr Kathryn Mannix’s book also and agree this conversation is needed. This blog will help others to make sense of this situation which was unfortunately experienced by many in the pandemic. Student Nurses and Educators will benefit from this and I will share widely. Best wishes, Maeve
Thank you for your kind words Maeve and for sharing the blog. It’s good to see that people are finding something useful here.
We’re increasingly adding useful resources to our blogs where we can. You may or may not have seen that every two months we do a blog that gathers up the latest Cochrane evidence relevant to nurses, along with opportunities/news/resources. We’re not sure whether people are finding these useful! But for now we are continuing with them and you can find them here, along with some relevant blogs on single topics https://www.evidentlycochrane.net/category/evidence-for-nursing/
Sarah
Beautifully and sensitively written, Sarah, and a very much needed resource. Thank you.
Thank you very much Karen.
We can add to the list of resources we’ve included here too, and I hope people will share any they’ve found helpful.
Sarah, this is such a beautifully written piece, and by sharing your personal story you will be supporting so many others to prepare and understand for z peaceful death. Thank you so much for this information. Our condolences again for the loss of your lovely mum.
Thank you so much Sandra.
Extraordinary indeed! Thank you Sarah for sharing your touching story and creating such an in-depth resource for people to use. I have aging parents and I hope we are blessed with our own Sylvia when the time comes – what a star!
Thank you Muriah. Sylvia was such a blessing. We are so grateful that, despite not being able to be with Mum, we felt that she lacked nothing at the end – and had a good death at home, just as she wished.