In this guest blog, pelvic physiotherapist and comedian Elaine Miller tells us what we need to know to avoid constipation and when the going gets tough.
Page last updated 23 January 2023
Constipation is a miserable condition which can worsen co-morbidities like low back pain, muscle tone problems in people with neurological conditions and confusion in people with dementia. It is therefore a condition that needs to be understood and managed – but there is a dearth of research to guide us.
One of the main issues is encouraging people to seek help. Many people are simply too embarrassed to see their GP about bowel problems, which is a problem because one of the signs of colon cancer is a disruption in habits which lasts for longer than three weeks.
Therefore, I don’t discourage poo talk from my children, not even in front of Grandma (though, I draw the line at “Last Christmas, I went for a poo, and the very next day, I flushed it away. This year, to save diarrhoea, I’ll eat up my grains and fibre…” <proud mum>). The children’s continence charity ERIC has excellent resources for parents and for professionals in health and education, to try and normalise toilet talk.
What is normal?
- When you first feel the urge to poo you can hold on long enough to get to a toilet without accident.
- You do a poo within a minute of sitting on the toilet, it doesn’t hurt, and you don’t have to strain.
- You completely empty your bowel, you don’t have to go back again, or have a feeling of some “left”.
- It is normal for you to feel an urge to poo within about half an hour of eating. This is the gastrocolic reflex and is what prompts people to want to go to the toilet in the morning. People’s normal pattern can range from several times a day to several times a week – it’s a good idea to pay attention to what your bowel habit is.
Here’s how it works
The indigestible parts of our food pass into the colon, which absorbs water and electrolytes. The large intestine is full of bacteria which change the food remnants into faeces. The time it takes for food to pass from one end of the digestive tract to the other is called “bowel transit time”, one to three days on average, and 90% of that time is spent in the bowel. A slow bowel transit time means the faeces spends longer in the large intestine becomes dehydrated and more difficult to pass.
The stool travels from the colon into the rectum, through the internal sphincter muscle and then through the external sphincter muscle on its way out of the anus. The internal sphincter muscle automatically relaxes the top of the anal canal, triggering nerves to signal that you need to go. The external sphincter is under voluntary control and can push the stool back out of the anal canal if there is nowhere suitable for us to go to the toilet. However, repeated withholding can cause constipation, particularly in children – it’s best to move your bowels when you feel the first urge.
Poo position


Why is straining bad?
Straining increases your intra-abdominal pressure and causes congestion of the soft tissues. So, you are more likely to develop piles, prolapse or vaginal varicose veins. Cases of people fainting or having heart attacks when straining are well known. Ask Elvis.
Also, we know that a full bowel can irritate a bladder – many cases of incontinence are related to constipation. In my experience, deal with the bowel first.
What about diet?
Government guidelines published last year say we should aim for 30g a day of fibre. The NHS website has some suggestions for how to get more fibre into your diet. Increase daily fibre gradually (5g a day) to avoid bloating. And, remember to drink plenty of water.
Bowel diary
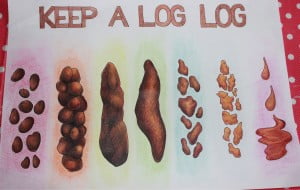
Adjust diet and fluid intake with the aim to be a 3-4 if you are prone to diarrhoea, a 4-5 if you are prone to constipation.
Massage
The first record of abdominal massage as a treatmentSomething done with the aim of improving health or relieving suffering. For example, medicines, surgery, psychological and physical therapies, diet and exercise changes. for chronicA health condition marked by long duration, by frequent recurrence over a long time, and often by slowly progressing seriousness. For example, rheumatoid arthritis. constipation was in 1870. Interest has resurfaced and we know it can help move stool along and relieve cramping or bloating symptoms. Many non-randomizedA non-randomised study is any quantitative study estimating the effectiveness of an intervention (harm or benefit) that does not use randomisation to allocate people to comparison groups. studies have suggested that it is an effective interventionA treatment, procedure or programme of health care that has the potential to change the course of events of a healthcare condition. Examples include a drug, surgery, exercise or counselling. for constipation and has no known side effects.
People can learn to self massage to good effect – and what mammal doesn’t like the idea of a tummy rub? Start on the right side by the hip bone. Rub in a circular motion up the right side to the rib cage, across the abdomen to the left side and then down to the left hip bone and across the pelvis to the umbilicus. Always massage in a clockwise direction as this is the direction of digestion.
Medication
Best get advice from your GP or pharmacist. For instance, we don’t want people buying themselves over-the-counter bulk forming laxatives if they have chronic constipation. If you are already bunged up, you don’t need any more volume.
Pregnancy, childbirth and bowels
Pregnancy is particularly challenging because the growing uterus squashes the colon and the hormonal changes make it sluggish. Many pregnant women are prescribed iron supplements which increase the riskA way of expressing the chance of an event taking place, expressed as the number of events divided by the total number of observations or people. It can be stated as ‘the chance of falling were one in four’ (1/4 = 25%). This measure is good no matter the incidence of events i.e. common or infrequent. of constipation. Fear of post-delivery pain from tear or episiotomy sites can cause anxiety around bowel movements.
These issues are often missed in antenatal appointments and classes because of time constraints. It is very important, however, that women get good information about good bowel management – particularly if she has had a tear or episiotomy. You are going to nurse that first postnatal poo along and have to resist the urge to put a bonnet on it and give it a name…(ask me how I know).
Worry and discomfort are going to have a negative impact on maternal happiness and breastfeeding. Improved education might reduce the need for medication in this populationThe group of people being studied. Populations may be defined by any characteristics e.g. where they live, age group, certain diseases.. Toilet straining places stress on pelvic tissues and is associated with vaginal prolapse, rectal prolapse and piles. None of which are remotely funny.
What does the research say?
Not an awful lot. Much of the research is poor quality and little of it includes the Bristol Stool Chart, measures of pain or quality of life.
This Cochrane Review on interventions for treating constipation in pregnancy (published September 2015) compared bulk forming with stimulant laxatives in pregnant women. DataData is the information collected through research. were poor but they concluded there was evidence that increasing fibre formed a better stool. The review states there is a need for further randomizedRandomization is the process of randomly dividing into groups the people taking part in a trial. One group (the intervention group) will be given the intervention being tested (for example a drug, surgery, or exercise) and compared with a group which does not receive the intervention (the control group). controlled trialsA trial in which a group (the ‘intervention group’) is given a intervention being tested (for example a drug, surgery, or exercise) is compared with a group which does not receive the intervention (the ‘control group’). (RCTs) in different settings with a range of types of laxative and measurements of pain as well as stools.

The authors of the Cochrane ReviewCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. Interventions for preventing postpartum [after childbirth] constipation were able to include just five trialsClinical trials are research studies involving people who use healthcare services. They often compare a new or different treatment with the best treatment currently available. This is to test whether the new or different treatment is safe, effective and any better than what is currently used. No matter how promising a new treatment may appear during tests in a laboratory, it must go through clinical trials before its benefits and risks can really be known. when they published the review in 2015 and found no more to add when they updated it in 2020. Again, reporting was poor and none of the trials included pain, straining, incidenceThe number of new occurrences of something in a population over a particular period of time, e.g. the number of cases of a disease in a country over one year. of constipation or quality of life. All trials did measure time to first bowel movement. They did not, however, record what the woman’s normal, pre-delivery pattern was. They recommended future trials should include behavioural and educational interventions and measure pain, straining and quality of life as well as time to first post-natal bowel movement.
Another CochRane review by the same team, looked at interventions for treating post-partum constipation (September 2014). They excluded nine studies on the basis that they did not meet the inclusion criteria and found none that they could include. They recommended rigorous and well conducted large RCTs.
There are some studies looking at adults with neurological problems, who often have problems with faecal incontinence or constipation. There are lots of papers examining the cause of neurogenic bowel disorders, but, few looking at the management of them. The Cochrane Review Management of faecal incontinence and constipation in adults with central neurological diseases (January 2014) included twenty trials, mostly poor quality, but they suggest that a good bowel routine (using laxatives, suppositories, enemas, diet, exercise and digital evacuation) is important and should be based on the needs of the individual. Massage and even one education session with a nurse may help reduce constipation, but more and better research is needed before we can say that with confidence. The reviewers commented that there was “remarkably little research on this common problem” and repeated the call for more, good, randomized studies.
Until that happens, we will all just have to continue trial and error. With our knees above our hips.
Top bowel tips
- drink plenty of water
- avoid caffeine
- eat fibre
- exercise
- go when you feel the first urge
- after breakfast, sit on the toilet for 15-20 minutes and wait for the ejection reflex- which does exactly what it says
- take your time on the toilet
- raise feet on a stool, lean forwards
- don’t hold breath, ssss, grrrr, or moo
- do a pelvic floor contraction when the bowel movement is done to encourage complete closing
- congratulate yourself on releasing the poo hostage
Editor’s note: The Cochrane Review Probiotics for treatment of chronic constipation in children (March 2022) found a lack of evidence on the effectivenessThe ability of an intervention (for example a drug, surgery, or exercise) to produce a desired effect, such as reduce symptoms. or safetyRefers to serious adverse effects, such as those that threaten life, require or prolong hospitalization, result in permanent disability, or cause birth defects. of probiotics used to treat chronic constipation without a physical explanation in children.
Join in the conversation on Twitter with @CochraneUK and @GussieGrips or leave a comment on the blog.
Please note, we cannot give specific medical advice and do not publish comments that link to individual pages requesting donations or to commercial sites, or appear to endorse commercial products. We welcome diverse views and encourage discussion but we ask that comments are respectful and reserve the right to not publish any we consider offensive. Cochrane UK does not fact check – or endorse – readers’ comments, including any treatments mentioned.
The featured image and the image of mother and baby have been purchased for Evidently Cochrane from istock.com and may not be reproduced. The sitting man and log log are Elaine’s work so do ask her if you want to use them.



[…] Cochrane Regno Unito notato che è necessario piegarsi in avanti sui gomiti per ridurre la necessità di sforzarsi. […]
[…] Cochrane UK noted you need to be leaning forward on the elbows to help reduce the need to strain. Your elbows […]
[…] Cochrane UK noted you need to be leaning forward on the elbows to help reduce the need to strain. Your elbows […]
[…] Cochrane UK noted you need to be leaning forward on the elbows to help reduce the need to strain. Your elbows […]
[…] Cochrane UK noted you need to be leaning forward on the elbows to help reduce the need to strain. Your elbows […]
[…] Evidently Cochrane: Easing the Strain: put your feet up for constipation […]
[…] Easing the strain: put your feet up for constipation […]
I am really benefited by this post and I got a chance to read it through Physiopedia Newsletter every Tuesday. Now I can give more better suggestions to my clients when they open up to me about Constipation issues. Thank you
I have learned that the single largest cause of constipation is that we don’t drink enough water! With this type of constipation, things worsen, as the stool stays longer than it should in the large intestine and more liquid is absorbed from it, making the constipation worse.
You did not mention natural stool softeners like mineral oil, which doesn’t get absorbed in the intestines, and therefore keeps the stool soft and easier to pass.
A great way to naturally help prevent constipation is to eat a orange every morning, even with the pith. This increases fiber in a natural way, and contains enough liquid to prevent the problems you could experience with fiber laxatives and not enough fluids.
Hi Elaine, how are you? Congratulations on the blog, I follow it weekly. I tried this procedure and it didn’t work for me. I’m so tired, I’ve tried so many supplements, meds and exercises. I was referred to a new prebiotic supplement do you think I should try it? I’m suffering a lot, I have nothing else to do, I stay for 1 week if I even go to the bathroom.
Hi Mary, We’re glad you follow the blog. I have taken the weblink out of your comment as we don’t allow links to commercial websites. Elaine is taking a break from social media while she is involved in an election campaign but you may wish to follow her on Twitter @GussieGrips or go to her website gussetgrippers.co.uk
Best wishes,
Sarah Chapman [Editor]
After reading this blog I can surely say that you have done a lot of research on this topic.
I like how you have mentioned the excellent tips to prevent constipation and its causes here.
I know many people who are unaware that constipation can be prevented because of this lack of knowledge, people tend to ignore it and have severe problems in their old age.
Anyways, there were many causes here that I was not aware of. It provided me with value.
Thank you again for writing on this. Highly appreciated.
Shitty article, but I rather enjoyed it atop the stool stool here in the old stool shed.
I am 63 years old and have had constipation since childhood. Nothing seemed to work, except at times some small amount of licorice used as a laxative. .Then my sister said: “when you are on the toilet, lean back a little, and lean to the left side, try that”. And it worked wonderfully. It could be a last tactic to use, yet I’m happy with this.
Fiber makes ALL the difference!
Have some soluble fibers. Try oats with hot water with some milk in the morning and your bowel movements will be the best thing in your life! The soluble fiber absorb water and add bulk and softness to your stool. Please try it.
Can you have constipation and diarrhea at the same time
Yes. If you are constipated, liquid stool may be able go around the “clog” so you are still constipated.
Hmm
So informative best I have ever read and great advice Thank you so much
I find sitting on my hands helps (hands under thighs) as you can rock yourself into different positions, thus making it easier to poop. Also just as you are about to start to lower yourself on to the loo, start pushing a little bit before you get to sitting position. It makes a big difference. Also always go when you get the first urge.
Lifting my legs and moving forward on the toilet, totally works. Feeling much better now 😁 Thank you so much 👍
I am 80 years old and I am having a prob with constipation just recently.i am drinking more water and I hope it will improve.
You may not need a stool. Lean forward and lean your body weight on tip toes. If position annoys your back, arch it if needed. That way you aren’t “carrying ‘two’ stools” to a restaurant restroom. Your tip toes do the job.
Very informative & great suggestions
I thought I was going to die ,I sent out Text to Ex wife forgiving and caring for i thought last moments of my life,,it was hard as a rock ,instead of toilet I poo on kitchen floor so 8 have counter to hold onto
Really, Really Thank You!!!!!!
I am having chronic constipation and this is so far the best articel I have read and thanks a lot, it’s has helped me a ton. Great wishes to this author!!!!!!!
This is the best piece of literature I have read in 60 years. It is so informative and straight forward. I am 70 years old and have sever different pooping problems. This will help me so much. Thank you!
You’ve never heard this one!!!!
I would like to know if there’s any research showing why I become so anxious when constipated—-now this is the most important part——doctors always say it’s because I’m anxious about not being able to go. THATS NOT IT!!! I know that’s not it cuz I can wake up in a full blown anxiety attack before I even know I have to go!! It seems there’s an area in my large intestine where once the poo gets past it – whether it comes out or not – once it gets past this certain spot my anxiety is alleviated- believe me it has nothing to do with my feelings about not being able to go. I think when I’m constipated for a long time the toxicity level raise and that is what causes the anxiety. what do you think
Crazy. I’m the same way!!
I have been reading a book by Dr Jolene Brighten called “Beyond the Pill”. It covers much more than that though and explains how food and lifestyle work with your body’s natural cycles. There is a chapter on gut health, which explains that you must “always be pooping” as otherwise the toxins (including hormones, caffeine, alcohol) that your liver has filtered out go back into circulation in your body if your bowel movements are too infrequent. This then leads to other health issues from an imbalance in these hormones/chemicals ranging from mood swings, anxiety, aggression, hair loss/gain and whatever those hormones are meant to do, but on overdrive as you now have too much. This could be what you’re experiencing with anxiety getting high after you haven’t pooped for a few days. Perhaps take a look at her research.
Good blog on constipation. As a licensed massage therapist I have done MANY stomach massages for my clients over the years. It truly helps! I would suggest people eat more plant based foods .. more smoothies , fresh juices, raw veggies and fruit to help get rid of constipation 😁
Good blog on constipation and what to do. As a massage therapist I swear by massages! They help all the impacted junk come out naturally. All my clients I have had who were constipated told me massage worked every time. 😃
Very precisely and informative written blog.
The blog has covered almost every aspect of healthy bowel.
Remember constipation can be the cause of dangerous piles,so if you notice anything uncommon in your bowel movements, do get it diagnosed.
Hello! This post could not be written any better!
Reading through this post reminds me of my old room mate!
He always kept chatting about this. I will forward this page to him.
Fairly certain he will have a good read. Thank you for sharing!
a brilliant article and a great combination of humour and fact – toilet humour at its best