In this blog for people interested in memory, thinking problems and dementia, Jodi Watt (a researcher at the University of Glasgow) looks at the latest Cochrane evidenceCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. on whether a class of commonly-used medications (anticholinergics) might increase people’s riskA way of expressing the chance of an event taking place, expressed as the number of events divided by the total number of observations or people. It can be stated as ‘the chance of falling were one in four’ (1/4 = 25%). This measure is good no matter the incidence of events i.e. common or infrequent. of future memory problems, or even dementia.
Blog last updated: 23 May 2023.
Take-home points
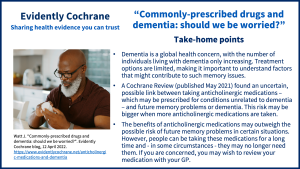
Currently, around 54 million people live with dementia globally, a number which is increasing as a result of the ageing populationThe group of people being studied. Populations may be defined by any characteristics e.g. where they live, age group, certain diseases.. TreatmentSomething done with the aim of improving health or relieving suffering. For example, medicines, surgery, psychological and physical therapies, diet and exercise changes. options for dementia are limited. As such, it is important to understand any factors which may lead to the development of future problems with memory and thinking.
Ultimately, for dementia, prevention is better than cure. Understandably there is a public appetite to know more about dementia risk factors and almost every week there is a new headline about a medication that may cause or prevent dementia.
A 2017 Lancet Report (discussed in a previous Evidently Cochrane blog Behind the headlines: can one in three dementia cases be prevented?) reported nine modifiable risk factors for dementia, with a further three suggested for addition in 2020. These are things people may be able to do something about, in order to reduce their risk of developing dementia – and many of them are lifestyle and environmental factors.
However, there is an absence of clarity around medication decisions which may also contribute.
What are anticholinergic medications, and what have they got to do with dementia?
Many day-to-day medications work by targeting the cholinergic system. The cholinergic system is a series of chemical signalling pathways within the body. Medications with anticholinergic effects block this signalling action, which can be helpful to control common medical conditions such as asthma, hayfever, and overactive bladder. Drugs that target this pathway are so important that many appear on the World Health Organization’s Model List of Essential Medications.

However, use of anticholinergic medications may come with risks.
Most importantly, drugs that block cholinergic pathways have been linked to memory and thinking problems (cognition), and even dementia. A link between disrupting cholinergic signals and dementia makes biological sense. The medications we use to treat the symptoms of dementia, like donepezil, enhance cholinergic signalling – so it is no wonder that we may be concerned about the brain health consequences of anticholinergics.
If anticholinergics cause lasting problems with memory and thinking, this probably doesn’t happen immediately. ‘Anticholinergic burden’ refers to the cumulative effect of these medications. It is unique to an individual based on their own historic and current use of anticholinergic medication.
The evidence for a relationship between anticholinergic burden and cognition
A Cochrane ReviewCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research., Anticholinergic burden (prognostic factor) for prediction of dementia or cognitive decline in older adults with no known cognitive syndrome (published May 2021), looked at all the published evidence exploring a link between these anticholinergic medications and future memory problems or dementia.
The review included 25 studies of 968,428 people with no memory or thinking problems, aged 50 years or older, who were followed up after at least one year. The review found that long-term use of anticholinergic medication may be linked to an increased risk of future dementia, and that this risk may be bigger when more anticholinergic medications are taken.
Specifically, the results of this review suggest the use of anticholinergic medications has the potential to double an individual’s risk of dementia. A doubling of risk sounds alarming but needs to be considered in context. For most healthy adults, dementia in the short term is unlikely. So, a doubling of this risk still represents only a modest overall risk of dementia. The same may not be true for people at higher risk of dementia, for example, older adults who already have issues with memory and thinking. This is a group where great care needs to be taken when considering whether to start or continue anticholinergic medications.
How good is this evidence?
The reviewers can only say that there may be a link.
The evidence from this review is ‘low certainty’, which means that conclusions could not be confidently made. Some reasons for this are that it is difficult to definitively say whether anticholinergic medications caused cognitive decline, or if other factors were responsible.
Additionally, comparing studies from different researchers can sometimes be tricky. In particular, ‘anticholinergic burden’ is measured by researchers on various scales, and this can result in differing scores that are difficult to compare between studies.
The people included in the studies often used multiple medications and it is likely that they may have health conditions that may co-occur with changes in cognition, making the true effect of the anticholinergic drugs difficult to disentangle from the effects of the conditions they were prescribed for.
Furthermore, some anticholinergic drugs may be prescribed for the early signs of dementia. For example, in the early stages of dementia people can have urinary problems that may be treated with anticholinergics. This can exaggerate the apparent associationA relationship between two characteristics, such that as one changes, the other changes in a predictable way. For example, statistics demonstrate that there is an association between smoking and lung cancer. In a positive association, one quantity increases as the other one increases (as with smoking and lung cancer). In a negative association, an increase in one quantity corresponds to a decrease in the other. Association does not necessarily mean that one thing causes the other. between these medications and dementia, but it may not be the medications causing the memory and thinking problems.
Where do we go from here?
Determining the true nature of a possible link between anticholinergic medication and dementia is challenging.
Ultimately, truly determining whether a causal link exists between anticholinergic burden and future dementia may require a long-term, large-scale studyAn investigation of a healthcare problem. There are different types of studies used to answer research questions, for example randomised controlled trials or observational studies. in which some people have their anticholinergic medications stopped or changed to alternatives, and others continue with their usual medications.
Doctors are certainly already cautious about prescribing these medications in older adults. Indeed, some guidelines (for example the NICE guidance on dementia) recommend a medication review to look for anticholinergics as part of the assessment of a person with memory concerns. This Cochrane Review may add to that caution. Nevertheless, sometimes the benefits of these drugs will outweigh the uncertain risk of future memory problems.
What if I am concerned about my own use of anticholinergic drugs?
It is important to remember that anticholinergic drugs are hugely important in the medical field, and they can be of real benefit to patients. Reviewing the use of these drugs is necessary though, as some people can be on anticholinergic drugs for a long time and may no longer need them. As with any medication that you have been on for a long time, it may be possible to stop anticholinergics. You should not abruptly stop any medications, but if you are concerned you should speak with your GP surgery about reviewing your medication use.
Join in the conversation on Twitter with @CochraneUK and @CochraneDCIG or leave a comment on the blog.
Please note, we cannot give specific medical advice and do not publish comments that link to individual pages requesting donations or to commercial sites, or appear to endorse commercial products. We welcome diverse views and encourage discussion but we ask that comments are respectful and reserve the right to not publish any we consider offensive. Cochrane UK does not fact check – or endorse – readers’ comments, including any treatments mentioned.
Jodi has nothing to declare.


