In this blog for both women with prolapse and healthcare professionals, Myra Robson, a pelvic health physiotherapist, looks at the latest Cochrane evidenceCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. on pessaries for pelvic organ prolapse and explores its impact on clinical practice.
Page last updated 31 August 2022 to add two Patient Decision Aids from NICE, which help you compare the treatmentSomething done with the aim of improving health or relieving suffering. For example, medicines, surgery, psychological and physical therapies, diet and exercise changes. options. Page checked 11 July 2023
Pessaries for pelvic organ prolapse are one of the most exciting inventions in pelvic health, in my opinion. Vaginal pessaries are passive mechanical devices that are worn internally. They are designed to support the vagina and hold the prolapsed organs back in the correct position. I see many women in my clinical practice who benefit from using pessaries, but it is so important to have evidence from research to direct our treatments and to understand both benefits and potential risks.
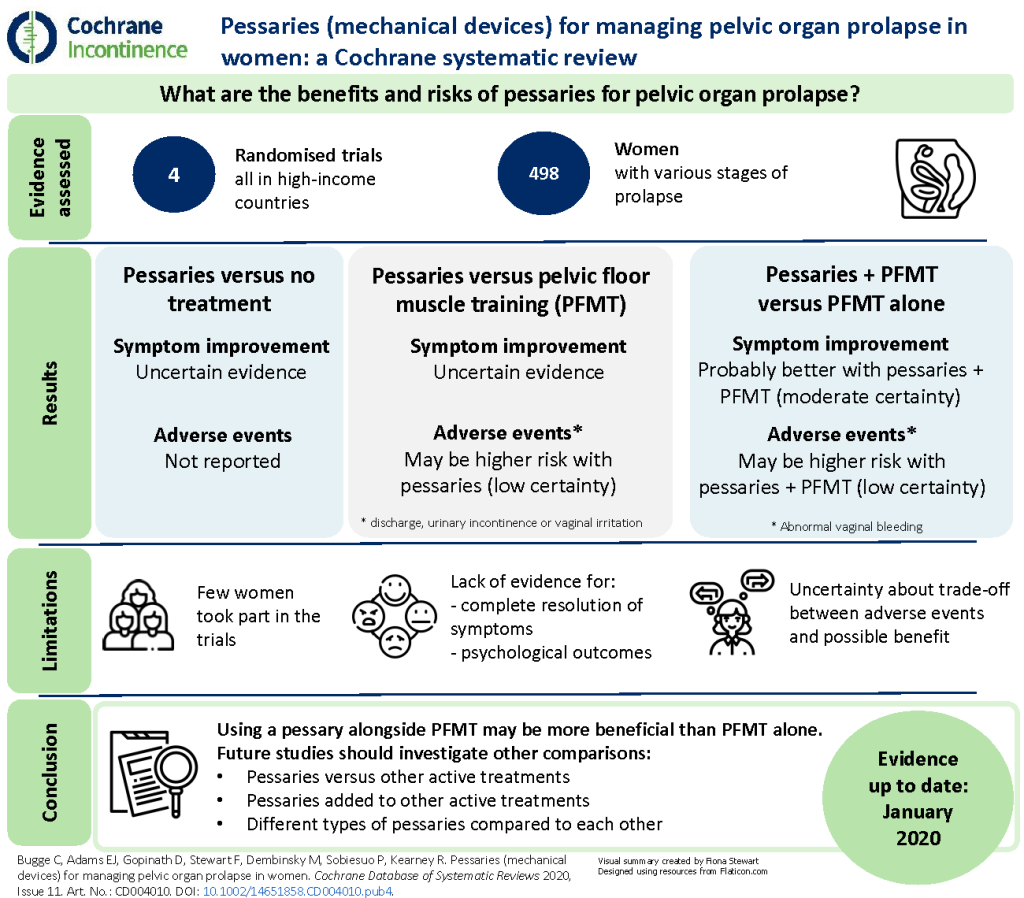
I welcomed the recent Cochrane ReviewCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research., Pessaries (mechanical devices) for managing pelvic organ prolapse in women (published November 2020) to add to our scant knowledge base.
As always with Cochrane, I was not disappointed in the review, although the evidence itself is still not as comprehensive as it could be. The evidence base is insufficient to strongly direct our treatments using pessaries, but it is a start.
What is a pelvic organ prolapse?
The Cochrane Review states that “Pelvic organs, such as the uterus, bladder or bowel, may protrude into the vagina because of weakness in the tissues that normally support them. This protrusion is known as pelvic organ prolapse. Women who experience prolapse report a wide variety of symptoms that affect their quality of life.”
Some key facts about pelvic organ prolapse:
- Common – 50% of women over 50 will have a prolapse
- Connected to a variety of factors e.g., childbirth, constipation, hyper-mobility, high BMI
- Life-changing and distressing for many women
- Low riskA way of expressing the chance of an event taking place, expressed as the number of events divided by the total number of observations or people. It can be stated as ‘the chance of falling were one in four’ (1/4 = 25%). This measure is good no matter the incidence of events i.e. common or infrequent. of serious issues e.g., urinary retention and ulceration in external prolapses
- Very high risk of secondary problems related to reducing exercise, especially high-intensity exercises beneficial for bone health
- Huge impact on quality of life
What does pelvic organ prolapse feel like?
- Lump, heaviness or dragging in the vagina
- A feeling of something “coming down”
- Discomfort in the perineum (the area between the anus and genitals)
- Lump in the vagina, coming outside of the body
- Urinary or faecal leakage
- Constipation or incomplete bowel emptying
- Hesitation in emptying the bladder
- Incomplete bladder emptying
- Backache
How is pelvic organ prolapse diagnosed?
As with many pelvic health concerns in women, it often is not diagnosed – either because women accept a variety of symptoms and just put up with it, or because the symptoms are subtle and changeable at times. Many women present after discovering a “lump” in the shower and panic that they may have cancer. Others are told that they have a prolapse during a smear test. Women rarely know about prolapse until it happens to them. It is a poorly understood condition for something that affects 50% of women!
Prolapse can be assessed and diagnosed by a GP, pelvic health nurse or physiotherapist, or gynaecologist. Diagnosis can be hard as a prolapse may not be obvious at 9am in the morning with empty bowels and lying flat on a couch, compared to 5pm in the afternoon – standing up with full bowels after a day of walking.
Diagnosis is therefore multi-factorial and the focus is on the symptoms that the women describe rather than on what healthcare professionals can see or feel.
How is pelvic organ prolapse treated?
Treatment falls into three broad areas, covered well in the NICE guidance: Urinary incontinence and pelvic organ prolapse in women: management:
- Lifestyle management and pelvic floor rehabilitation
- Pessaries
- Surgery
Lifestyle management includes:
- Weight loss
- Optimising defecatory techniques
- Bladder and bowel training
- Dietary advice
- Pelvic floor exercises
- Adaptations to sport and daily activities
- Supportive sportswear
- Topical oestrogens to supply oestrogen to the vaginal area post-menopause or in some breastfeeding women*
- Lots of reassurance and explanation!
Pessaries
- More in a moment…
Surgery
It is beyond the scope of this blog to delve into this but I will make two key points:
- Firstly, surgery is complex for many reasons. We know that there is approximately a 20-30% chance of prolapse coming back following surgery for prolapse and so it cannot be considered a guaranteed complete cure.
- Secondly, women should always be referred for physiotherapy to support their pelvic floor management before having surgery as this allows time to prepare for the operation and make sure that pelvic floor function is maximised.
Back to pessaries…
The Cochrane Review states that “Vaginal pessaries are one treatment option for prolapse that are commonly used to restore the prolapsed organs to their normal position and hence relieve symptoms. A vaginal pessary can be used to treat all four prolapse stages.”
This is a well-designed summary that puts over the incredibly important point that a pessary may work at any stage for any prolapse! I have heard the following statements so many times over the years:
- Your prolapse is too mild for a pessary
- Your prolapse is too severe for a pessary
- You are too young for a pessary
- You are too old for a pessary
- You can’t have sex if you use a pessary
Interestingly, no-one who makes these claims can ever define what the right age, prolapse or stage is!
The evidence for pessary management is limited, coming from four studies with just 478 women with various stages of prolapse, and most of it has been assessed as ‘very low-certainty’ and therefore unreliable.
The review authors concluded that:
“We are uncertain if pessaries improve pelvic organ prolapse symptoms for women compared with no treatment or when compared to another active treatment like PFMT”.
However, they did find moderate-certaintyThe certainty (or quality) of evidence is the extent to which we can be confident that what the research tells us about a particular treatment effect is likely to be accurate. Concerns about factors such as bias can reduce the certainty of the evidence. Evidence may be of high certainty; moderate certainty; low certainty or very-low certainty. Cochrane has adopted the GRADE approach (Grading of Recommendations Assessment, Development and Evaluation) for assessing certainty (or quality) of evidence. Find out more here: https://training.cochrane.org/grade-approach evidence that pessaries in addition to PFMT probably improve women’s symptoms and prolapse-specific quality of life. But there may be an increased risk of abnormal vaginal bleeding with pessaries compared to no treatment or PFMT.
This finding is absolutely in line with my experiences and clinical practice and is a good start to developing the evidence base to support working with this patient group. Let’s look at these points in a little more detail. (You can also view a visual summary of the review at the bottom of this blog).
Do pessaries work?
- Prolapse is all about what the women feels, not what we see. As healthcare professionals, if the woman in front of you says that a certain pessary works and allows her to reach her goals, then it works! The Cochrane authors call for future studies to measure women’s perceived resolution of prolapse symptoms.
- Pessaries should be used alongside pelvic floor exercises, rehabilitation as appropriate, lifestyle management and goal-specific strategies (Urinary incontinence and pelvic organ prolapse in women: management, 2019)
What are the potential harms?
The Cochrane authors say that it would be helpful to have some research into women’s experiences of the unwanted effects reported in existing research studies. The review found that there may be an increased risk of unwanted effects with pessaries compared with no treatment or PFMT. In my experience, risks are very low indeed if a pessary is properly managed and if a topical oestrogen is used. Patient understanding and compliance is important, and appropriate follow-up care is likely to reduce risk considerably, and pick up on any issues at an early stage. Issues may include:
- Discomfort
- Erosion
- Vaginal discharge
- Embedding if completely forgotten about
- Impact on bladder and bowel function
Why do we not use them more?
Pessaries are poorly understood and frequently used badly. I could discuss this for a long time, but I will go to my favourite way of explaining how we should use pessaries and why we go wrong so often.
Finding a pessary that fits is a bit like shoe shopping…
Imagine the average woman going to Marks and Spencer’s for a pair of shoes. This is like a woman going to a clinic for a pessary.
Now imagine her trying on two pairs of black, high-heeled, pointy shoes in a size 6 and size 7. One is too big and one is too small (the 6.5 is out of stock), black is not suitable for the wedding she is attending, she can’t walk in heels and the pointy bit hurts. She asks for help and is told “Sorry, madam, shoes are obviously not right for you.”
Logic would suggest that she tries all the sizes, along with different styles. The assistant should be clear about what she needs the shoes for and measure her feet to give her a good start… the woman and assistant need time, space, privacy, a good selection of footwear, and so on.
Women are often presented with one or two options of pessary when the variety is huge. The fitting process is fraught with problems, and there are not enough fitters. I could go on and on… but I am running out of space!
Where does this leave us?
We now have a clear summary of the limited evidence available and know where the gaps are. From my perspective as a pelvic health physiotherapist, it backs up what I have thought for some time. We know we need more evidence to guide us on pessary use. In the meantime, we need to use pessaries with the excellent clinical reasoning we already possess. We need to use a variety and avail ourselves of the experts in the field who can teach us so much. We need, most of all, to listen to women.
Talking to your GP about pelvic organ prolapse
If you are a woman who has pelvic organ prolapse, here are some pointers that could help you discuss treatment options with your GP:
- Keep a diary of your symptoms – when they come on, what makes them worse etc.
- Take a photo of any bulge, if it is not there consistently
- Think about your needs and goals – are you a runner or weight lifter? Are you a carer who needs to lift? Do you stand in your job?
Sources of further information and support
- www.thepogp.co.uk – Pelvic, Obstetric and Gynaecological Physiotherapy AssociationA relationship between two characteristics, such that as one changes, the other changes in a predictable way. For example, statistics demonstrate that there is an association between smoking and lung cancer. In a positive association, one quantity increases as the other one increases (as with smoking and lung cancer). In a negative association, an increase in one quantity corresponds to a decrease in the other. Association does not necessarily mean that one thing causes the other.
- Pessaries and pelvic organ prolapse support group – Facebook
- NICE (National Institute for Health and Care Excellence) Patient decision aids:
.
Editor’s note, July 2023: The authors of a Cochrane Review Oestrogen therapy for treating pelvic organ prolapse in postmenopausal women (July 2023) conclude that “we are uncertain about the effects of oestrogen therapy on pelvic organ prolapse in postmenopausal women”.
Join in the conversation on Twitter with @CochraneUK and @C_Incontinence or leave a comment on the blog.
Please note, we cannot give medical advice and do not publish comments that link to individual pages requesting donations or to commercial sites, or appear to endorse commercial products. We welcome diverse views and encourage discussion but we ask that comments are respectful and reserve the right to not publish any we consider offensive. Cochrane UK does not fact check – or endorse – readers’ comments, including any treatments mentioned.
Myra Robson has nothing to disclose.



Great piece. The UK Guideline launched in March 2021 also a good resource to mention for women and clinicians https://thepogp.co.uk/patient_information/womens_health/pessaries_for_prolapse.aspx and on the UKCS website: https://www.ukcs.uk.net/UK-Pessary-Guideline-2021