In this blog for people looking to reduce their chances of catching colds and flu this winter Robert Walton, a very general practitioner, looks at Cochrane evidenceCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. on probiotics, an increasingly popular and natural way of trying to reduce the riskA way of expressing the chance of an event taking place, expressed as the number of events divided by the total number of observations or people. It can be stated as ‘the chance of falling were one in four’ (1/4 = 25%). This measure is good no matter the incidence of events i.e. common or infrequent. of upper respiratory infections such as colds, flu and infections of the throat, nose and sinuses.
Take-home points
A little yoghurt maker sat on the shelf above our washing machine unused for at least thirty years. The bright orange base of this family heirloom spoke to its design in the more flamboyant times of the early 70’s and brought me hope of better things to come during the first Covid lockdown.
Yoghurt making in England waned in popularity together with bell bottomed trousers. But we should perhaps refresh this skill in the light of a recent Cochrane ReviewCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. Probiotics for preventing acute upper respiratory tract infections (published August 2022) which looked at how probiotics – live bacteria commonly found in fermented foods such as yoghurt – can help to protect against a wide range of respiratory infections.
What are the benefits of probiotics?
Probably less likely to get respiratory infections
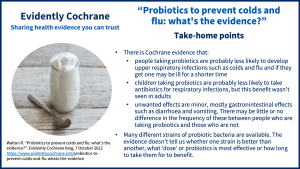
The results of the review were pretty surprising. The bottom line is that both adults and children taking probiotics are probably less likely to get upper respiratory infections – essentially coughs and colds – than people who are not taking them.
The review authors found that out of a thousand people, around 76 people taking probiotics (this could be as few as 49 people or as many as 117) would be expected to have three or more respiratory infections compared to 129 people not taking probiotics.
Probably less likely to need antibiotics for respiratory infections
Perhaps more importantly, among people taking probiotics, fewer would need to take antibiotics for their respiratory infection. Out of a thousand people, between 42 and 81 of the people taking probiotics would use antibiotics compared to 100 not taking probiotics. When the review authors looked at the evidence on adults and children separately, this benefit was seen only in children.
Governments and health systems worldwide are worried about frequent use of antibiotics which leads to resistance in the bacteria that cause illness. So any treatmentSomething done with the aim of improving health or relieving suffering. For example, medicines, surgery, psychological and physical therapies, diet and exercise changes. that reduces the need to use these important and sometimes lifesaving drugs is clearly a tremendous benefit to society.
Probiotics may shorten the length of the illness
Further good news was revealed when the Cochrane authors looked at how long the respiratory illness suffered by people taking part in the studies lasted. Those taking the probiotics may have been ill for about a day less than those who did not take probiotics.
Are there any side effects of probiotics?
And so far as side effects go there may be little or no difference in frequency between those who use probiotics and those who do not. Side effects were minor, mostly gastrointestinal problems like diarrhoea and vomiting. It’s rare to find an effective treatment that carries little risk of unwanted effects and this could make the probiotics particularly useful as a way of avoiding respiratory illnesses.
So how do you take these probiotics?
Children taking part in the studies usually took the bacteria in milk-based food of some kind and adults in powder-like food, although they were also used in drops and sprays. Generally, probiotics were taken regularly over the course of three to six months and the benefits were seen with both low and high doses.
The strains of bacteria used in the studies were mainly lactobacilli of the type used to make yoghurt although the particular subtypes may not be exactly those found on the shelves in ‘live yoghurt’ sold in supermarkets. It would be interesting to know whether one bacterial strain was better than another at preventing illness and intuitively one might think that would be the case. But in fact there is no evidence presented in the review to show which strain is best or what ‘dose’ and duration is most effecive.
And the yoghurt maker with the bright orange base? Well I took it down from the shelf and dusted it off looking for relief from lockdown boredom. The yoghurt maker performed perfectly keeping the milk at exactly the right temperature without the benefit of a microchip, LED display or even I suspect a transistor! The machine brewed a delicious batch of yoghurt and has been doing so every week or two since then. Colds and flu are thing of the past in my family …….. I wish!
Link:
Zhao Y, Dong BR, Hao Q. Probiotics for preventing acute upper respiratory tract infections. Cochrane Database of Systematic ReviewsIn systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. 2022, Issue 8. Art. No.: CD006895. DOI: 10.1002/14651858.CD006895.pub4.
Join in the conversation on Twitter with @rtwalton123 @CochraneUK or leave a comment on the blog.
Please note, we cannot give specific medical advice and do not publish comments that link to individual pages requesting donations or to commercial sites, or appear to endorse commercial products. We welcome diverse views and encourage discussion but we ask that comments are respectful and reserve the right to not publish any we consider offensive. Cochrane UK does not fact check – or endorse – readers’ comments, including any treatments mentioned.
Robert Walton has nothing to disclose.



The author’s clear and concise presentation of the research findings makes it accessible to a wide audience, fostering a better understanding of the topic. This article not only highlights the importance of maintaining a healthy balance of gut bacteria but also encourages a proactive approach to immune health. Kudos to the author for shedding light on this fascinating and relevant area of research!
[…] 2 . Walton R. “Probiotics to prevent colds and flu: what’s the evidence? ” Evidently Coch… […]
[…] 2 . Walton R. “Probiotics to prevent colds and flu: what’s the evidence? ” Evidently Cochrane… […]