Sarah Chapman blogs about a Cochrane rapid review produced in response to the COVID-19 pandemic, looking at the evidence on convalescent plasma as a possible treatment for COVID-19. This blog discusses a living systematic review, which was last updated on 01 February 2023.
Page last updated 03 February 2023.
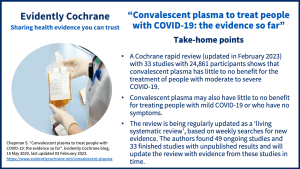
In response to the COVID-19 pandemic, Cochrane has been producing rapid reviews. These are simplified systematic reviews that can be done in a few weeks to produce timely evidence for decision-making. One of these, Convalescent plasma or hyperimmune immunoglobulin for people with COVID‐19: a living systematic review, updated on 1st February 2023, brings together the evidence on convalescent plasma as a possible treatment for people with COVID-19.
What is convalescent plasma?
Plasma is a liquid that makes up about half of your blood volume. After a person has recovered from an infection (this is the convalescent bit), their blood contains antibodies that help fight infection. Some people who have fully recovered from an infection can donate plasma (as with blood donation, there are reasons why they might not be able to). Randomized trials are being done to investigate the potential benefits or harms of using plasma from people who have recovered from COVID-19 to treat people who are currently ill with it.
Convalescent plasma has been used in the past to effectively treat infections where there were no drug treatments or vaccines, such as diptheria and polio. Evidence on whether it helps treat severe respiratory infections has been mixed and there are potential harms too, such as allergic reactions.
This has led some researchers to consider plasma as a potential treatment for COVID-19, but we need to know what evidence there is on the benefits and risks.
What is the evidence from the Cochrane Rapid Review?
The review authors looked for studies investigating convalescent plasma for people with COVID‐19, without any limits on age, ethnicity, gender or disease severity.
The latest news (01 February 2023)
This review is being updated as a ‘living systematic review’. The authors search for new evidence every week and update the review when they identify relevant new evidence.
In February 2023, the review was updated for the fifth time. The review now includes 33 studies with 24,861 participants (29 of these studies included people with moderate to severe COVID‐19; the other four included people with mild COVID‐19). The studies mainly took place in hospitals, in countries all over the world.
Plasma as a treatment for people with moderate to severe COVID‐19
Compared to placebo or standard care, convalescent plasma makes little to no difference to:
- the chance of dying from any cause up to 28 days after treatment
- needing invasive mechanical ventilation
- being discharged from hospital
Convalescent plasma probably makes little to no difference to serious unwanted effects, and may make little or no difference to quality of life.
Plasma as a treatment for people with mild COVID‐19
Compared to placebo or standard care, convalescent plasma may make little to no difference to:
- the chance of dying from any cause up to 28 days after treatment
- admission to hospital or death within 28 days after treatment
- the time until COVID‐19 symptoms resolve
- serious unwanted effects.
Certainty that plasma has little to no benefit for treating people with moderate to severe COVID-19
The latest update of this review has brought increasing certainty. We can be confident that convalescent plasma has little or no benefit as a treatment for people with moderate to severe COVID‐19 – and that it may have little or no benefit for people with mild COVID-19 or who have no symptoms.
More studies under way…
The authors found 49 ongoing studies and 33 finished studies with unpublished results. They will update the review with evidence from these studies as soon as possible. Hopefully, new evidence may answer the remaining questions, particularly about people with mild COVID-19.
What about antibodies made in a laboratory?
Plasma contains naturally-produced antibodies, but antibodies can also be made in a laboratory, from cells taken from people who have recovered from the disease. These can be made to target only one specific protein – in this case, a protein on the virus that causes COVID‐19. These are called ‘monoclonal antibodies’. They attach to the COVID‐19 virus and stop it from entering and reproducing in human cells. This may help to fight the infection. It is thought that they might cause fewer unwanted effects than convalescent plasma, which contains a variety of different antibodies.
A Cochrane Review SARS‐CoV‐2‐neutralising monoclonal antibodies for treatment of COVID‐19 (published September 2021) explored the potential benefits and harms of laboratory-made monoclonal antibodies. It included 6 studies with 17,495 people (some of whom were hospitalised, others were not).
Overall, the “current evidence is insufficient to draw meaningful conclusions” about whether monoclonal antibodies are an effective and safe treatment for COVID-19. However, there are 36 ongoing studies which will hopefully address this uncertainty.
For more information, you can listen to this Cochrane podcast: Are laboratory-made, COVID-19-specific monoclonal antibodies an effective treatment for COVID-19?
Read these Cochrane Clinical Answers:
- For adults with asymptomatic or mild COVID‐19, what are the effects of SARS‐CoV‐2‐neutralising monoclonal antibodies (alone or combined)?
- For adults hospitalized with moderate to severe COVID‐19, what are the effects of SARS‐CoV‐2‐neutralising monoclonal antibodies (alone or combined)?
On this page, which is constantly updated, you can stay informed about Cochrane content relating to the coronavirus (COVID-19) pandemic and the various related activities that Cochrane is undertaking in response.
Join in the conversation on Twitter with @CochraneUK @SarahChapman30 or leave a comment on the blog. Please note, we cannot give medical advice and we will not publish comments that link to commercial sites or appear to endorse commercial products.
Sarah Chapman has nothing to disclose.



Seeing as the antibodies in people who have recovered from Coronavirus, whether they were very ill or whether they were asymptomatic should be found in the plasma, maybe we should consider making vaccines out of the blood of people who have recovered, the same way they have used horses and eggs to build vaccines for other conditions.
It may be a bit late when someone is already sick to be able to see the difference. People are not knock-off rats, so it’s hard to get a good comparison, especially when hospitals are overworked. Conditions such as hyperglycemia upon entering the hospital would have to be matched, and which combination of ApoE genes.
What about using convalescent plasma on healthcare workers and others who have an exposure to COVID-19, such as the San Jose Kaiser Permanente first responders?