In a blog for people with ear-related balance disorders and those supporting them, Sarah Chapman and Selena Ryan-Vig from Cochrane UK share the latest Cochrane evidenceCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. and some useful resources, introduced by Professor Martin Burton.
Featured image: ‘Spinning Down’ by Catherine Duggan. With permission via Ménière’s Society.
In this blog, we include information about the following:
- vestibular migraine
- persistent postural perceptual dizziness (PPPD)
- Ménière’s disease
- unilateral peripheral vestibular dysfunction
- motion sickness
In this way, a distinguished neurologist introduced a chapter on giddiness in a much-used textbook of neurology. Such a reaction is due mainly because it can be so difficult to diagnose some balance disorders, and difficult to treat them. The physicians are frustrated not to be able to help their patients more easily. But dizziness or giddiness is common, and sometimes the cause is identifiable and sometimes the cause lies in the patient’s ear or ears. A number of Cochrane reviewsCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. looked at some of these. – Professor Martin Burton.
1
Vestibular migraine
Vestibular migraine is a type of migraine that comes with attacks of vertigo or dizziness. Other symptoms of migraine often go with it, such as headache, sensitivityA measure of a screening or diagnostic test’s ability to correctly detect people who have the disease. to light/noise, nausea/vomiting and visual changes.
A team from Cochrane has looked for the best available evidence on medication and on other ways to prevent vestibular migraine, and on medication to treat it, publishing three new Cochrane Reviews in April 2023. These have all highlighted a lack of reliable evidence and this is something to be aware of when making choices about treatments.
Preventing vestibular migraine
Their review Pharmacological interventions for prophylaxis of vestibular migraine shows there is very little evidence on the effects of medicines for preventing vestibular migraine, so it is unclear whether they are helpful and whether they are likely to have unwanted effects.
There is also uncertainty about the potential benefits and harms of non-drug approaches to preventing vestibular migraine, such as changes to diet or lifestyle, as shown by the Cochrane Review Non‐pharmacological interventions for prophylaxis of vestibular migraine.
Treating vestibular migraine
There’s also an evidence gap on Pharmacological interventions for acute attacks of vestibular migraine, and it’s not clear whether any medications are effective for treating vestibular migraine. While there was little information available on harms of treatmentSomething done with the aim of improving health or relieving suffering. For example, medicines, surgery, psychological and physical therapies, diet and exercise changes. for this review, the use of triptans for other conditions (such as headache migraine) is known to have some unwanted effects.
Experiencing vestibular migraine
Writer Lydia Ruffles has given a powerful account of her experiences of vestibular migraine in her blog for Wellcome – Migraine, creativity and me.
2
Persistent postural perceptual dizziness (PPPD)
Persistent postural‐perceptual dizziness (PPPD) is a chronicA health condition marked by long duration, by frequent recurrence over a long time, and often by slowly progressing seriousness. For example, rheumatoid arthritis. balance disorder, characterised by subjective unsteadiness or dizziness that is worse on standing and with visual stimulation (for example, from complicated patterns or busy moving images). It was only recently defined and not much is known about how best to treat it. Two Cochrane Reviews, published in March 2023, have looked for evidence on medication and on other treatments for PPPD.
Medication to treat PPPD
Medication used to treat PPPD includes drugs known as ‘selective serotonin reuptake inhibitors’ (SSRIs) and ‘serotonin and norepinephrine reuptake inhibitors’ (SNRIs). The authors of the Cochrane Review Pharmacological interventions for persistent postural‐perceptual dizziness (PPPD) looked for evidence on the effects of these but found NO studies that could be included. So we don’t know whether they are helpful or harmful for the treatment of PPPD.
Alternatives to medication for PPPD
There was just one very small studyAn investigation of a healthcare problem. There are different types of studies used to answer research questions, for example randomised controlled trials or observational studies. to include in the Cochrane Review on Non‐pharmacological interventions for persistent postural‐perceptual dizziness (PPPD), on transcranial direct current stimulation, and no conclusions can be drawn from it. So we don’t know whether any non‐drug treatments may be helpful for the treatment of PPPD or whether they may have any potential harms.
3
Meniere’s disease
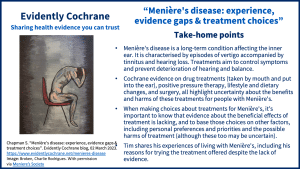
Cochrane has recently published six reviews on treatments for Meniere’s disease. Unfortunately, the reviews highlight uncertainty about the benefits and harms of drug treatments (taken by mouth and put into the ear), positive pressure therapy, lifestyle and dietary changes, and surgery. You can read more in our blog Menière’s disease: experience, evidence gaps & treatment choices. As well as looking at the evidence on treatments, the blog includes one person’s experiences of living with Menière’s and making choices about treatments, and reflections from two of the review authors.
4
Unilateral peripheral vestibular dysfunction
Unilateral peripheral vestibular dysfunction (UPVD) can happen because of disease, trauma or after surgery. It is characterised by dizziness, visual or gaze disturbances and problems with balance. It is managed with medication, physical manoeuvres and exercise regimes, the latter known collectively as vestibular rehabilitation.
The vestibular system includes the parts of the inner ear and brain that help process sensory information involved in controlling balance. Vestibular rehabilitation may be offered to people with any of a range of conditions characterised by unilateral peripheral vestibular dysfunction.
The authors of the Cochrane Review Vestibular rehabilitation for unilateral peripheral vestibular dysfunction (published January 2015) explain that “Components of vestibular rehabilitation may involve learning to bring on the symptoms to ‘desensitise’ the vestibular system, learning to coordinate eye and head movements, improving balance and walking skills, and learning about the condition and how to cope or become more active.”
The review authors conclude that “there is moderate to strong evidence that vestibular rehabilitation is a safe, effective management for unilateral peripheral vestibular dysfunction, based on a number of high‐quality randomisedRandomization is the process of randomly dividing into groups the people taking part in a trial. One group (the intervention group) will be given the intervention being tested (for example a drug, surgery, or exercise) and compared with a group which does not receive the intervention (the control group). controlled trialsA trial in which a group (the ‘intervention group’) is given a intervention being tested (for example a drug, surgery, or exercise) is compared with a group which does not receive the intervention (the ‘control group’).”.
They also found that vestibular rehabilitation probably resolves symptoms and improves functioning in the medium term. But for people with benign paroxysmal positional vertigo (BPPV), the evidence suggests that physical (repositioning) manoeuvres are more effective in the short term than exercise‐based vestibular rehabilitation; although a combination of the two is effective for longer‐term functional recovery.
5
Motion sickness (travel sickness)
Also known as travel sickness, motion sickness is common. In a short blog, GP Robert Walton looks at the Cochrane evidence on treatments: Treatments to prevent travel sickness: a quick look.
More information and support
- Meniere’s Society – Vestibular Disorders
- The Migraine Trust: Vestibular Migraine
‘Dizziness and Me’ artwork
Thank you to Lorraine Brookes, Catherine Duggan, Therese Guy and the Ménière’s Society for permission to use their artwork. Do visit the ‘Dizziness and Me’ collection to see more, and to submit your own artwork about your experiences of chronic dizziness.
Join in the conversation with @CochraneUK @SarahChapman30 or leave a comment on the blog.
Please note, we cannot give specific medical advice. We do not publish comments that link to individual pages requesting donations or to commercial sites, or appear to endorse commercial products. We welcome diverse views and encourage discussion. However, we ask that comments are respectful. We reserve the right to not publish any we consider offensive. Cochrane UK does not fact check – or endorse – readers’ comments, including any treatments mentioned.
Sarah Chapman and Selena Ryan-Vig have nothing to disclose.