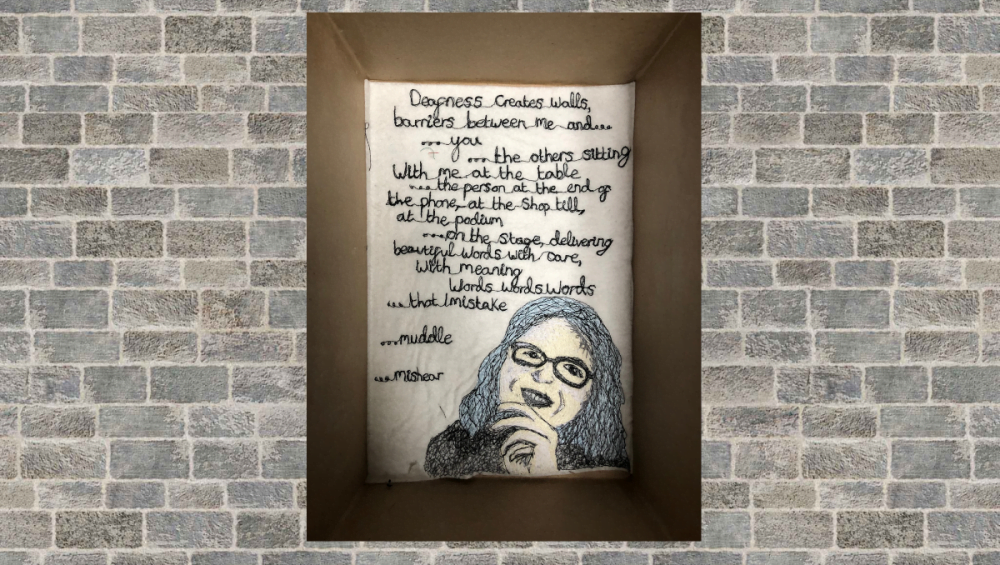
In this blog for adults with hearing loss, Dr Adele Horobin, Patient and Public Involvement and Engagement Manager at the Nottingham Biomedical Research Centre discusses COACH, a new clinical trialClinical trials are research studies involving people who use healthcare services. They often compare a new or different treatment with the best treatment currently available. This is to test whether the new or different treatment is safe, effective and any better than what is currently used. No matter how promising a new treatment may appear during tests in a laboratory, it must go through clinical trials before its benefits and risks can really be known. aiming to find out if hearing aids or a cochlear implant is better for adults with severe hearing loss – (long read). Featured image: ‘Deafness creates walls’ by Emily Chapman. Emily created this piece of textile art using some of the words her mother, Sarah Chapman, had used to describe her experiences of deafness.
Editor’s note February 2023: The COACH trial is recruiting people to take part. Could this be you? Find out more on the COACH Trial website and in this blog Cochlear implant or hearing aids? A clinical trial needs you.
Hearing loss – a long term condition that affects many people
We are facing a pandemic… a different pandemic. A pandemic that is often overlooked. More than 20% of the world’s populationThe group of people being studied. Populations may be defined by any characteristics e.g. where they live, age group, certain diseases. (nearly 1.6 billion people or 1 in 5 of us) are living with some form of hearing loss.1 Over 60% of people with hearing loss are over the age of 50.1 Hearing loss is only likely to increase as our world population ages – in 2018, for the first time in history, persons aged 65 years or over worldwide outnumbered children under age five.2 By 2050, it is projected that 2.45 billion people will be living with hearing loss. These are scarily high figures.1
So, what can we do about it? Raising awareness of safe listening (limiting exposure to sounds that are loud enough to damage the ears), increasing investment in hearing health care, childhood screening, better management of common conditions such as otitis media (glue ear) and more widespread vaccination programmes (a number of infectious diseases can affect hearing) can all help. Improving hearing device technology and the ways in which we use that technology also plays a big role too.
What is it like to have hearing loss?
That may not be as straightforward as you imagine. It is not just that everything becomes a bit quieter. Hearing at some frequencies (or pitch) may be more impaired than at others. One ear may be more deaf than the other. And many people with hearing loss experience tinnitus (like ringing or buzzing in the ears). There are many implications for work and socialising too, particularly listening to something like speech in a noisy background. Hearing loss makes it tiring to listen and can affect one’s mental health too.
There are hearing loss simulators out there. There are examples of tinnitus sounds on the British Tinnitus Association website. Simple Misunderstanding, an art installation by Ben Glover, provides a virtual reality environment to replicate the struggles and difficulties that deaf people face every day.
Hearing aids and cochlear implants
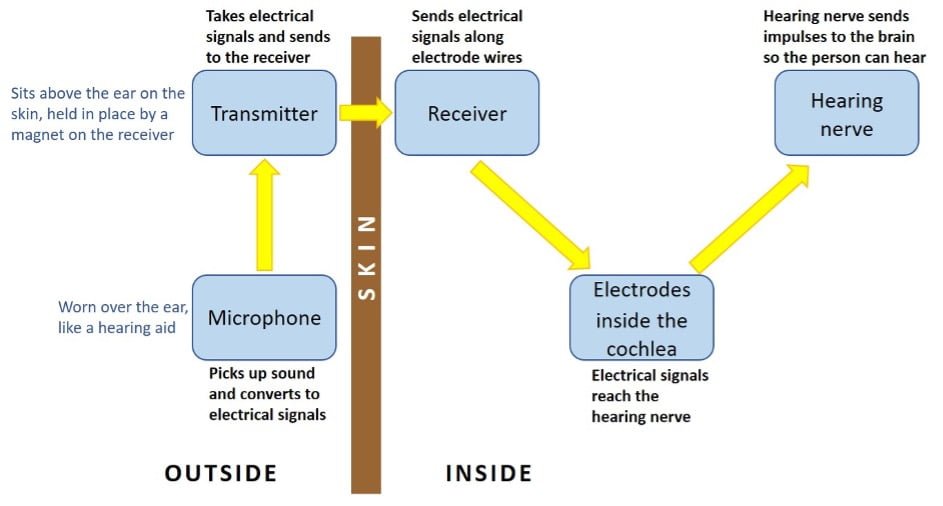
Conventional hearing aids have been the mainstay of hearing loss treatmentSomething done with the aim of improving health or relieving suffering. For example, medicines, surgery, psychological and physical therapies, diet and exercise changes. for many years. Relatively speaking, cochlear implants* are the ‘new kids on the block’, first used in the 1980s in the UK and not funded by the NHS until the mid 90s.3 As such, we still have a lot to learn in terms of who can benefit from them. Economics aside – cochlear implants are expensive! – this is reflected in the differing practices between countries as to who is offered an implant.
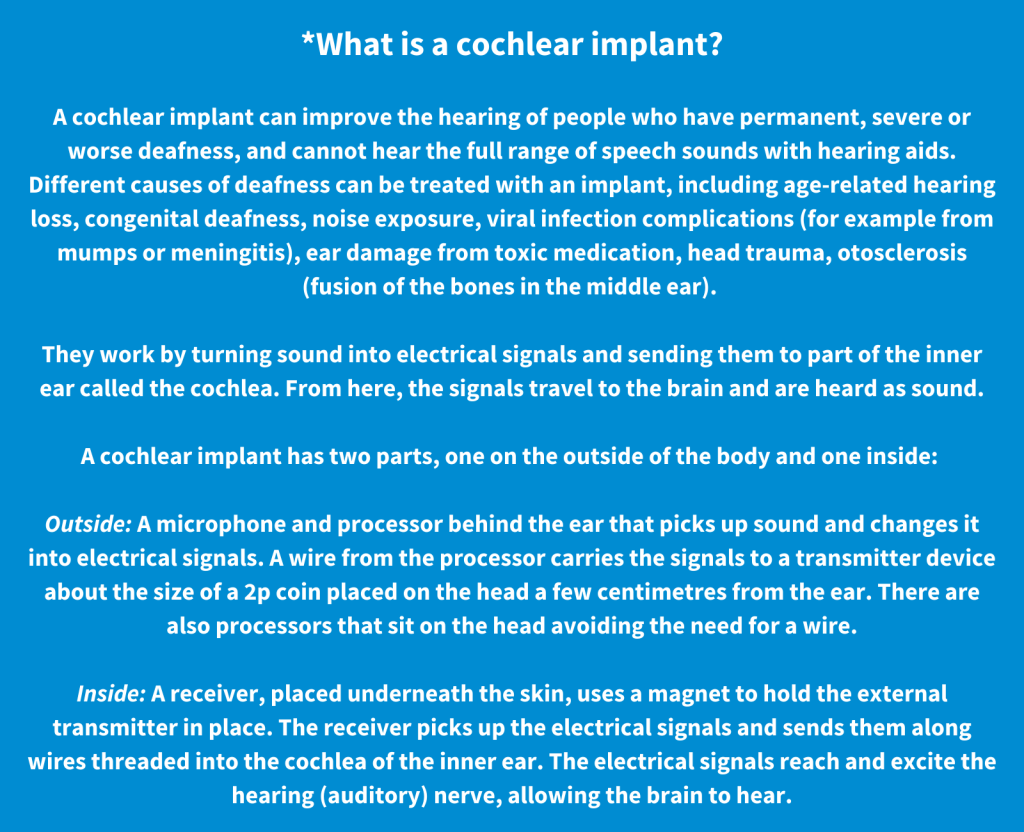

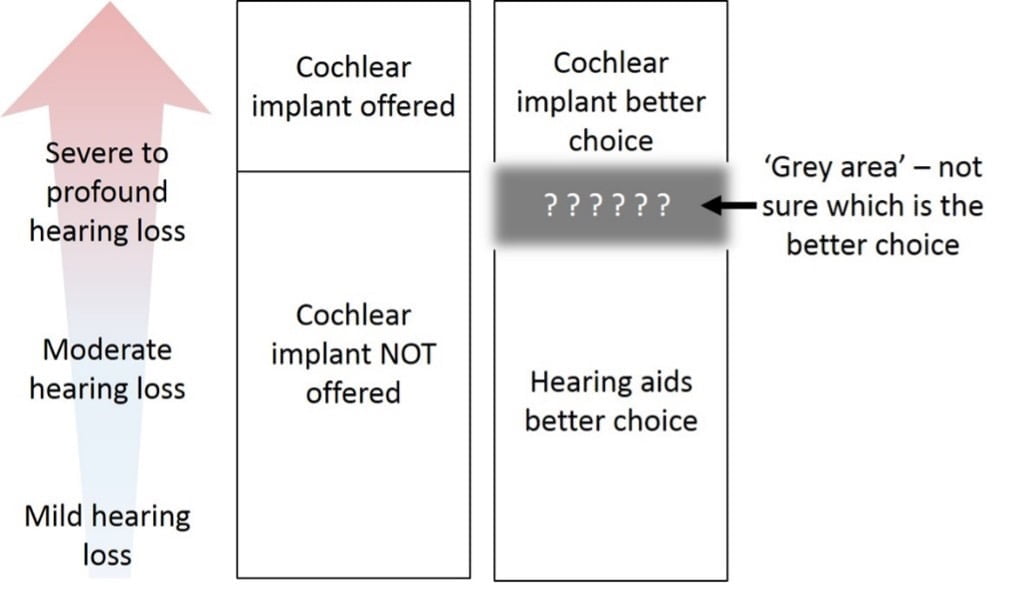
Cochlear implantation is recognised as a suitable treatment for severe to profound hearing loss. But guidance on just how severe hearing loss has to be in order for a person to be considered for an implant varies between countries.
At what point does a cochlear implant offer better hearing than hearing aids? The research evidence is not conclusive, in that when we compare the results of different trials, we are left uncertain as to whether a cochlear implant would outperform hearing aids in people who can hear sounds quieter than 80 decibels. This uncertainty is reflected in current guidelines from The UK’s National Institute for Health and Care Excellence (NICE).4 These state that patients who can only hear sounds louder than 80 decibels (about as loud as an alarm clock or kitchen blender) may be considered for an implant. But what about people who have slightly better hearing than that? Could they benefit from an implant, or would they be better with hearing aids? This is the ‘grey area’ that we wish to find answers to through a new clinical trial called COACH: A randomised controlled trialA trial in which the people taking part are randomly divided into groups. A group (the intervention group) is given the intervention being tested (for example a drug, surgery, or exercise) and compared with a group which does not receive the intervention (the control group). of cochlear implantation versus hearing aids in adults with severe hearing loss.
Are hearing aids or a cochlear implant better than the other?
In the COACH trial, researchers from the National Institute for Health Research (NIHR) Nottingham Biomedical Research Centre and the University of Nottingham Clinical Trials Unit are working with audiologists, surgeons and members of the public with severe hearing loss.
Involving people with lived experience of hearing loss
It is just as important to involve people in the team who live with hearing loss as it is to involve research and clinician specialists. Experts by lived experience, our public members offer a unique perspective on the impact of hearing loss and in the thoughts and decisions that come into play when making choices about using hearing aids and cochlear implants.
Di Matthews is a cochlear implant user who has been involved in the studyAn investigation of a healthcare problem. There are different types of studies used to answer research questions, for example randomised controlled trials or observational studies. from the start and is a member of the trial management group. She says: “I’ve had progressive hearing loss since I was 20 in the days of analogue hearing aids. Technology with hearing aids and cochlear implants has improved tremendously. However, we need to know where the criteria ultimately should start for a cochlear implant. For me a cochlear implant has vastly improved my quality of life, but I was implanted under the old 90 decibel criteria. If there had been more research and evidence, would I have benefitted earlier? We need this trial to determine which treatment is the best option for a wide range of individuals within a grey area. If you fall in the grey area, please get in touch to find out more, or to receive updates and share the evidence upon completion.”
Our new Patient Ambassador for the trial, Sarah Chapman says “I’ve lived with progressive hearing loss all my adult life. Now at the point where I often struggle to understand speech with the best hearing aids I can have, I am waiting to have a cochlear implant (I’m blogging about my cochlear implant journey, and living with hearing loss, in my personal blog From Ear To Eternity). If I get the improvement in my hearing that I hope for, I might wish I’d been able to have an implant years ago, when my hearing was in the ‘grey area’ that Adele talks about here. But the reality is that we don’t know how hearing aids and cochlear implants compare for people at this level of hearing, just above the current eligibility criteria. Finding this out is really important, to guide the allocation of precious resources, and to enable people to make informed choices about treatment. The COACH trial will address this gap in the evidence. The COACH team recognise the importance of inviting people with lived experience of hearing loss to contribute their expertise to many different aspects of the design and running of the trial, and I am really looking forward to getting stuck in as Patient Ambassador.”
We also have a public research partners advisory group, members of whom have been advising the team on what is important to our potential research participants and how best to communicate the trial to them. They will continue to be involved in the trial as it is set up and will be of vital help in supporting participantA person who takes part in a trial, often but not necessarily a patient. recruitment, creating patient-facing material, giving a patient viewpoint on the dataData is the information collected through research. analysed and in sharing results. Stuart Bunton is a member of the advisory group. He says “I’m a hearing aid wearer because I have been hard of hearing since birth and rely a lot on lip reading. This project has given me a great opportunity to be involved in how hard of hearing people struggle in the world of noise. For myself, I don’t know what it sounds like to hear birds chirping and have a ‘normal’ conversation round a table. Cochlear implants for the ‘grey area’ is important research as I have never been approached about the idea of a cochlear implant throughout my regular hearing check-ups.”
Two members of the public with lived experience of a cochlear implant or hearing aids are also member of our trial steering committee which provides independent oversight and governance.
Launching a trial to address uncertainty
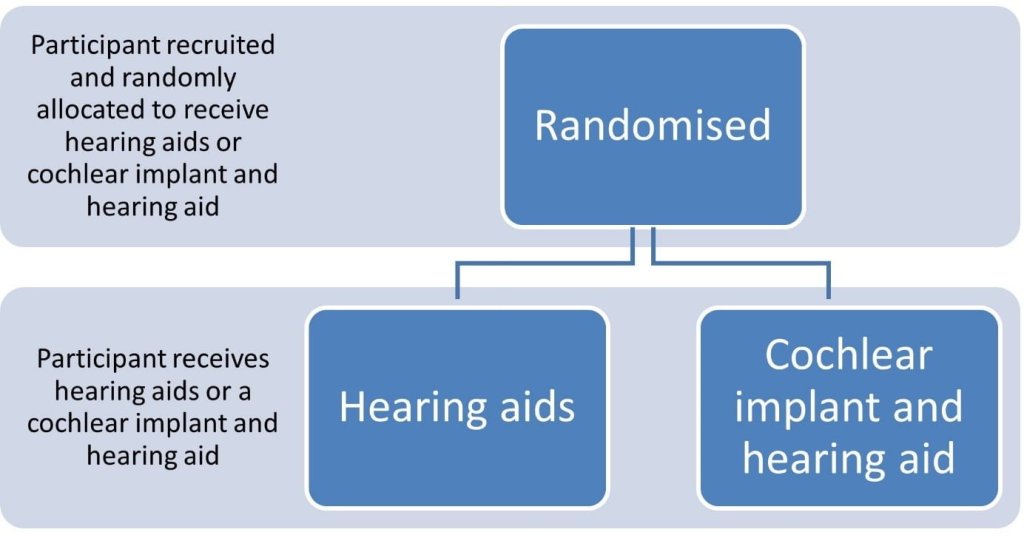
In the COACH trial, participants will have a 50:50 chance of being offered up to date hearing aids (or optimising their existing aids, whichever they prefer) or a cochlear implant as well as a hearing aid for the ear that is not implanted.
Regardless of which option they receive, they will be offered support and monitoring. We will test how well they can understand speech in quiet surroundings using their devices and then compare the results. We will also test the effects of their devices – cochlear implant and/or hearing aids – on broader hearing-related aspects. This includes listening to speech in noisy backgrounds, difficulties listening in everyday environments, listening-related fatigue, and tinnitus. We will also explore the effect of cochlear implantation more broadly, on wellbeing and quality of life. Any safetyRefers to serious adverse effects, such as those that threaten life, require or prolong hospitalization, result in permanent disability, or cause birth defects. aspects of cochlear implantation in comparison to hearing aids will be recorded as well.
This trial will give us the evidence we need to help patients, healthcare providers and practitioners decide between cochlear implants and hearing aids. Results will also feed into future reviews of NICE eligibility criteria.
Why can’t we offer everyone a cochlear implant?
Many of you reading this may have twigged that hearing aids are more readily available on the NHS, so it is likely that our trial participants would have been offered hearing aids already but may be willing to consider an implant. So why can’t we offer all participants an implant, to give them a new option? Well, that comes down to the concept called ‘equipoise’. This is where, according to available research evidence, we are genuinely uncertain as to which treatment is better. This means that we really don’t know whether hearing aids or a cochlear implant is the better option for patients who have hearing loss which is severe but not severe enough to qualify for a cochlear implant according to current national NICE guidance. Ethically, we could only offer the choice of a cochlear implant to all trial participants if we knew this was the better option. And if we knew this, we wouldn’t need a clinical trial to find out the answer. While newer technology may naturally appear to be the better option, this isn’t always the case, and it may be no better or even worse!
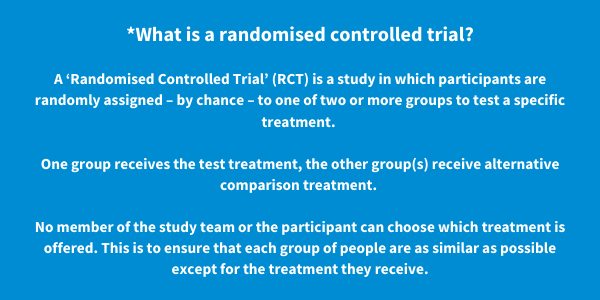
We need to conduct reliable, high-quality research to test whether a treatment is a suitable option for specific groups of patients. A randomised controlled trial is regarded as one of the most reliable and strongest forms of research evidence. Through the COACH trial, we hope to clear up this uncertainty so we can be sure that patients in the future will be offered the most appropriate treatment, whichever that might be.
Who is funding and running this trial?
This study is funded by an industry grant awarded to the University of Nottingham from Cochlear Ltd, a company who make cochlear implant devices. But it is run by NHS Doctors, NHS Audiologists, and researchers from the University of Nottingham, without the company being involved. The University’s contract with the funder makes sure that the funder cannot influence the conduct of the trial, data analysis or publication of results. The study is led by Dr Padraig Kitterick of the University of Nottingham and the NIHR Nottingham Biomedical Research Centre. A team of people are managing the study with Padraig.
How do I find out more?
Want to keep in touch with developments, including when we start recruiting participants? Please join our mailing list at: https://mailchi.mp/d4d0fff4a40f/coach to receive updates.
More about hearing conditions
On this page Hearing conditions: evidence, experience and resources (March 2023) we share trustworthy evidence and resources about hearing conditions and highlight opportunities to take part in research. Our blogs help to set evidence in context and make it easy to understand, and often include reflections from people living with hearing conditions and from health professionals and researchers.
Read the rest of the blogs in our ‘Living with Long-Term Conditions’ series.
Join in the conversation on Twitter with @COACH_trial @CochraneUK or leave a comment on the blog.
Please note, we cannot give medical advice and do not publish comments that link to individual pages requesting donations or to commercial sites, or appear to endorse commercial products. We welcome diverse views and encourage discussion but we ask that comments are respectful and reserve the right to not publish any we consider offensive. Cochrane UK does not fact check – or endorse – readers’ comments, including any treatments mentioned.
Adele Horobin has nothing to disclose.


Hi, this is a really good article. The trial is really interesting. My husband is on a waiting list for CI. He has otosclerosis, his left ear is completely deaf and right ear is severely hearing impaired and relies on hearing aid. He has been a hearing aid wearer for at least 20 years but never qualified for CI. He has struggled and has been unable to go out. We struggled as a family also. I pushed for CI contacting charities and he is now on the waiting list. We would be interested in contributing to your study if he qualifies when he gets his CI.