In a blog for anyone making health decisions, big or small, Sarah Chapman looks at some key things that can help you make a choice that feels right for you and reduce the riskA way of expressing the chance of an event taking place, expressed as the number of events divided by the total number of observations or people. It can be stated as ‘the chance of falling were one in four’ (1/4 = 25%). This measure is good no matter the incidence of events i.e. common or infrequent. that you’ll regret your choices later on. Included here are links to good resources and to some of our blogs in which people have discussed their health decisions and shared things that helped them.
Cochrane UK hosted a free webinar on Thursday 20th October 2022 on Making health decisions, with patients and doctors reflecting on their experiences and some important things to consider when making health decisions. The recording is available here.
Page updated 26 June 2023.
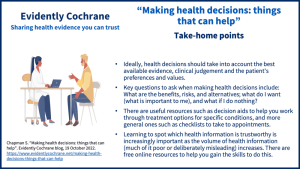
Take-home points
We all make health decisions. Some of these might be about trying to stay well: whether to buy those vitamins, for example, or take up that invitation for a vaccination. Some will be about how to deal with minor ailments, while others may be complex decisions about managing serious illness or long-term conditions.
The costs may be limited to time or money spent on treatmentSomething done with the aim of improving health or relieving suffering. For example, medicines, surgery, psychological and physical therapies, diet and exercise changes. but for others, they might be more far-reaching. Some decisions affect other people around us, adding to the complexity. What can we do to reduce the risk of regretting our decision later, especially when the stakes are high? What can we do to feel, at the time and later, and if people question our choices or the outcomeOutcomes are measures of health (for example quality of life, pain, blood sugar levels) that can be used to assess the effectiveness and safety of a treatment or other intervention (for example a drug, surgery, or exercise). In research, the outcomes considered most important are ‘primary outcomes’ and those considered less important are ‘secondary outcomes’. isn’t all we hoped, that we made the best choice we could at the time? We’ll be talking about this during the webinar, but here are some things that can help.
Ask 3 questions (for starters)
- What are my options?
- What are the pros and cons of each option for me?
- How do I get support to make a decision that is right for me?
Researchers have found that when patients Ask 3 Questions their clinicians provide better information about treatment options.
NHS Inform (Scotland) has a handy checklist you can use to get the most out of your healthcare appointments: It’s okay to ask.
There may be specific question prompts and checklists relevant to your health condition. Lara Cowpe, in her blog Talking to GPs about endometriosis: Lara’s story, mentions resources from Endometriosis UK to help you prepare for Visiting your doctor, which includes a downloadable pain and symptom diary. She discusses making decisions in partnership with her GP, and includes tips for people preparing to visit theirs, as well as things she’d like GPs to know.
I’ve written about the questions I thought might be useful to ask, and the things I weighed up in making my decision about whether to have a cochlear implant, in this blog: Discussing cochlear implants with a surgeon.
For Karen Morley, seeking help for Obsessive Compulsive Disorder, finding some relevant Cochrane evidenceCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. was key to feeling in control and to having a fruitful discussion with a GP about the way forward. You can read about this in her blog My OCD story: evidence-based medicine to the rescue and, in My OCD story part 2, how – four years on – she has become a more confident partner in making shared decisions about her health.
Which brings us to….
Evidence, and learning to spot which health information is trustworthy and which isn’t
Cochrane has worked with Lifeology to produce a free flashcard course – What is an infodemic and how can we prevent it? – that walks the reader through practical tips to combat misinformation and to think critically about health information.
Tips for deciding if information is credible, included in the course, include fact-checking claims by looking for it in different sources like government and research organization websites, and asking:
- Who wrote or said this?
- Are they providing research and stats? Are they telling me where they got this information?
- What’s the purpose of this content? How does it make me feel?
- Could this be biased? Is it news or an opinion? Does it provide both positives and negatives? Pros and cons?
- Is this well written or designed? Does it have typos or look amateur?
- When was it published?
Our Health, Our Knowledge is a free, trustworthy and evidence-based online course specifically for people making health choices. It’s clear to follow and illustrates the points with examples and stories.
The Cochrane Library is one source of evidence that is free from conflicts of interest and provides the “stack of evidence from multiple research studies and clinical trialsClinical trials are research studies involving people who use healthcare services. They often compare a new or different treatment with the best treatment currently available. This is to test whether the new or different treatment is safe, effective and any better than what is currently used. No matter how promising a new treatment may appear during tests in a laboratory, it must go through clinical trials before its benefits and risks can really be known.” (in its systematic reviewsIn systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research.) that the Lifeology course points out is more reliable than single studies. It’s free to access for anyone in the UK (and in many other parts of the world). Cochrane ReviewsCochrane Reviews are systematic reviews. In systematic reviews we search for and summarize studies that answer a specific research question (e.g. is paracetamol effective and safe for treating back pain?). The studies are identified, assessed, and summarized by using a systematic and predefined approach. They inform recommendations for healthcare and research. each have a plain language summary which aim to make the evidence accessible to the general reader, and their evidence may be shared in other formats too, such as podcasts and blogs.
Cochrane Evidence Essentials is a free online course introducing health evidence and how to use it to make informed health choices.
iHealthFacts is a web page where you can submit a question about a health claim. to experts in health evidence at the University of Galway.
Evidence synthesis: what is it and why do we need it? is a short video introducing you to this topic.
Dr Lynda Ware shares some useful tips in this Evidently Cochrane blog Health advice in the media: how do we know what to believe.
If you’ve already found some evidence that seems to be relevant to your health situation, your doctor (or other health professional) should be happy to discuss it. But without any prior knowledge, you could ask what the evidence is for any options proposed, including the option of doing nothing – or not yet.
Decision aids
Decision aids are evidence-based tools that can help you work through treatment options.
The National Institute for Health and Care Excellence (NICE) has patient decision aids for a range of conditions, available from their page on Making decisions about your care.
NHS England has a range of decision support tools for specific health conditions, including cataracts, glaucoma and atrial fibrillation.
Ottawa Personal Decision Guides are designed for any health-related or social decisions and are available in several languages.
Our blog Heavy periods: evidence to help you weigh up treatment options highlights some questions you may wish to consider and discuss with a healthcare professional and includes a link to a NICE decision aid. There is also a decision aid on the page Featured Review: Interventions available during pandemics for heavy menstrual bleeding: an overview of Cochrane reviews.
Think BRAIN
This is a useful framework for weighing up a possible treatment choice:
What are the Benefits, Risks, Alternatives, what do I want and what if I do Nothing? These are good questions to ask yourself and discuss with your healthcare professional.
You can see how these elements looked for me when I was deciding whether to have a cochlear implant in the video about my decision, below.
Choosing Wisely Shared Decision Making Resources for both patients and clinicians include a leaflet for patients with questions that can help them make the right choices for them, and use a version of this framework.
Some of our short blogs use BRAIN: on salt substitutes, cataract surgery and treatments for vaginal thrush.
Making decisions for other people
Making health decisions for others for whom we have responsibility can weigh heavily. Many people have shared their stories in the comments on our blog Living and dying well after stroke and tell of agonising over decisions they had to make on behalf of a loved one unable to make it for themselves.
In the blog Informed decision-making” “we can” doesn’t mean “we should” I reflect on how I navigated a health decision for my Mum, who had dementia, with the help of geriatrician Kit Byatt, who gives some really useful information for making decisions for or with others.
In Tube feeding for people with dementia: making decisions, Charlotte Squires – a doctor in older adult care – reflects on options for supporting patients with severe dementia and their families, including issues around decision-making. Charlotte says that useful information can be found on these pages on Talking about death and dying and How do I make an Advance Decision (Living Will)?
Clearly documenting personal wishes in advance can be helpful in terms of care planning for any individual. For information about advanced care planning, and also Power of Attorney, see the Compassion in Dying website.
Paediatric intensive care doctor Rufaro Ndokera will be co-facilitating our webinar on making health decisions, and we hope we will have a blog from her on making decisions for children.
Honest communication
We all need honesty from our doctors (and other health professionals), including about uncertainties. This is a huge topic and we hope to add more resources about this as well as a blog about communication across different areas of healthcare. To start with:
In our blog Glioblastoma: honest conversations for shared decision-making Peter Buckle, a patient advocate whose wife died of glioblastoma, and Professor Scott Murray, GP and palliative care innovator, call for honest communication between health professionals and people with glioblastoma and their families, enabling shared decision-making and planning, with a focus on quality of life. They give sources of information and support for patients and families, and practical suggestions for clinicians.
We have included some useful resources about honest conversations and more in the blog Talking about dying: better conversations at the end of life.
There is an excellent resource on Improving news delivery in ultrasound, which has suggestions that could be adapted for other contexts.
Other resources
NICE also has a Shared decision making guideline for healthcare professionals and people using services (published June 2021)
The NHS website and Patient.info include information about a wide range of conditions, symptoms and treatments
Ten health literacy principles cancer patients need to know (published October 2022)
You can join in the conversation on Twitter with @SarahChapman30 @CochraneUK or leave a comment on the blog.
Please note, we cannot give specific medical advice and do not publish comments that link to individual pages requesting donations or to commercial sites, or appear to endorse commercial products. We welcome diverse views and encourage discussion but we ask that comments are respectful and reserve the right to not publish any we consider offensive. Cochrane UK does not fact check – or endorse – readers’ comments, including any treatments mentioned.
Sarah Chapman has nothing to disclose.


The health care
landscape is shifting from a focus solely on treatment to a more comprehensive approach that includes prevention and proactive management. Preventive measures such as vaccinations, regular check-ups, and screenings are becoming central in minimizing the occurrence of diseases. Technology is revolutionizing healthcare delivery, from telemedicine making services more accessible to data analytics helping in personalized treatment plans.
It’s great to see evidence-based information being shared in a clear and accessible way. I completely agree that considering personal values and preferences is key when making health choices. Keep up the good work, and I look forward to more insightful posts like this in the future! Cheers!
Briefly. The seminar on decision making was excellent. BRAIN is a great mnemonic. Ii just wanted to add a brief story about surgery and diverticulitis.
30 years ago after several wrong diagnoses, my horrible symptoms were described as “severe acute diverticulitis with adhesions”. Sigmoidoscopy followed plus extended X-rays. Drastic surgery ( removal of transverse, descending and sigmoid colon planned).
However, there was a 6 month waiting list. In the meantime, for different reasons, I visited an acupuncturist. She remarked on my skin condition and said I had a yeast infection. She said no yeasty foods, no sweet foods for a week. ALL my diverticulitis symptoms disappeared. 30 years later, no surgery, colon intact. Still avoiding yeast, chillies and chick peas. The surgeon was utterly uninterested in the reason for my improvement and decision not to have the surgery.
This is such a valuable piece, is there a downloadable option please?
We’re very glad you think it’s useful! There isn’t a downloadable version, but you’ll find all the resources in the references PDF at the end, which you could download. You could also print it of course. We update the blogs and will hope to add to this one with more good resources. We’ll also add a link to the webinar on making health decisions, which is taking place tonight and will be recorded.
Best wishes,
Sarah Chapman